FA GI Topics
Small Intestinal diseases
The Bottom Line
In the field, if you see a cow with signs of colic, or you can palpate small intestinal distention on rectal then proceed with an abdominal exploratory. Abdominal exploratory is an excellent diagnostic test. Identification of a lesion allows better decision making. If treatment is an option then referral is recommended, although the decision is often euthanasia. Remember you cannot visualize all parts of the bovine gastrointestinal tract and cannot follow it from duodenum to rectum! However, if you can’t visualize it, you can’t readily fix it either.
General Considerations
Causes of small intestinal gastrointestinal obstruction include luminal obstruction (both intraluminal such as blood clots and extraluminal such as adhesions), intussusception (more common in Brown Swiss), volvulus (more common in young cattle) and strangulation (eg from an adhesion, entrapment in a hernia).
Cattle have a short mesentery. Since mesenteric traction is very painful, exteriorizing the small intestine may lead to the cow lying down during a standing procedure. Be cautious of this when exteriorizing the small intestine during exploratory. Lidocaine can be injected into the mesentery if needed.
Pain- Cattle do not show colic signs in most gastrointestinal disorders. If you see a cow kicking at her belly or acting uncomfortable, it generally indicates a need for abdominal exploratory.
Rectal Palpation: Depending on where the obstruction is, you may or may not feel distended loops of small intestine. It is very difficult to differentiate between causes of small intestinal obstruction on palpation alone. If you do feel small intestinal distension, an exploratory is warranted.
Ping: Right Paralumbar Fossa. Depending on the extent of SI involvement, cattle may have abdominal distention in the right paralumbar fossa (right sided apple).
Clinical Pathology: With lesions leading to outflow obstruction and sequestration of fluid in the abomasum and rumen you will see a hypokalemic, hypochloremic metabolic alkalosis with elevated rumen chloride levels. Additional electrolyte abnormalities include hyponatremia, hypocalcemia. Chronic cases can result in a paradoxical aciduria (poor prognosis). If the cow has ischemic necrosis and peritonitis then they will shift to a metabolic acidosis with a relative hyperkalemia and CBC will have an inflammatory leukogram with left shift (poor prognosis). In the field, we often do not do blood work but have clinical signs of dehydration and shock (cold ears or extremities). Knowledge of the suspected electrolyte and metabolic abnormalities allows for prompt stabilization or accurate assessment of prognosis.
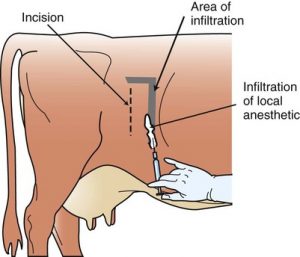 Surgical Approach: Right paralumbar fossa for surgical exploratory and visualization of the SI (best approach for most parts of the GI tract). Standing surgery using good surgical technique, local anesthesia and/or epidurals, and injectable analgesics (Banamine, butorphanol, and/or xylazine) provides a safer alternative to general anesthesia. In referral centers, we may opt to do general anesthesia in cases where there is a high risk for the cow to go down, but remember, laying a cow down for general anesthesia presents a very high risk due to regurgitation, pressure on their lungs from bloat, and myopathies.
Surgical Approach: Right paralumbar fossa for surgical exploratory and visualization of the SI (best approach for most parts of the GI tract). Standing surgery using good surgical technique, local anesthesia and/or epidurals, and injectable analgesics (Banamine, butorphanol, and/or xylazine) provides a safer alternative to general anesthesia. In referral centers, we may opt to do general anesthesia in cases where there is a high risk for the cow to go down, but remember, laying a cow down for general anesthesia presents a very high risk due to regurgitation, pressure on their lungs from bloat, and myopathies.
 Enterotomy: Can use a standing right paralumbar approach for this procedure. Exteriorize the portion of the small intestine and determine if the intestine is viable. If it is, make your incision on the antimesenteric side and remove the foreign body or blood clot. Close the enterotomy site with a two-layer closure using a simple continuous followed by a Lembert or Cushings to provide a water tight seal.
Enterotomy: Can use a standing right paralumbar approach for this procedure. Exteriorize the portion of the small intestine and determine if the intestine is viable. If it is, make your incision on the antimesenteric side and remove the foreign body or blood clot. Close the enterotomy site with a two-layer closure using a simple continuous followed by a Lembert or Cushings to provide a water tight seal.

Resection and Anastomosis: These are incredibly difficult to do in the field as the cow will often go down during the procedure. Referral is recommended for a cow who requires a resection and anastomosis.

