Equine Oral, Esophageal and Rectal disorders
Jaw fractures

Rostral mandibular and incisive fractures are common in horses and are actually readily managed in the field, despite their apparent complexity and stress level to the owners. [Jaw fractures in cattle are much less common!] Due to the type of forces placed upon the jaw and the excellent vascularity of the region, fractures involving the incisor region and interdental space generally heal rapidly and well following wire fixation.
These fractures are generally due to trauma and can occur in any age group. The most commonly affected group seems to be young males that are biting something when they get startled. Alternatively, kick wounds are common causes of unilateral fractures. Incisive fractures may involve only the alveolar bone of a single tooth. Fractures of the horizontal ramus of the mandible are invariably open and most often bilateral. Affected horses may drool saliva mixed with blood, have a protruded tongue and possibly an obvious deviation to the jaw. Maxillary fractures may be associated with additional head trauma. Mandibular vertical ramus fractures are rare and generally due to direct trauma.
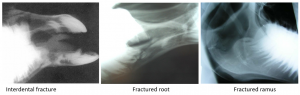
Oral examination is often more informative than radiographs; however radiographs are useful to identify tooth damage and fractures of the vertical ramus.
Several methods are employed to repair more extensive or vertical ramus jaw fractures, including plates, pins, and external fixateurs. However, due to the location of tooth roots, wire fixation is usually the preferred method for rostral fractures. Preoperative diagnostics should include a good oral examination to determine if any teeth have been damaged or if there is any risk of more caudal fractures. Radiographs are ideal but may not be necessary in many cases. Preoperative antibiotics are usually given and continued postoperatively. Anti-inflammatory drugs are helpful in speeding the animal’s return to a good appetite.
Incisive alveolar bone fractures

Occasionally just the labial plate of the alveolar bone is fractured, rather than the mandible. These may be replaced into the socket (adult teeth) or removed (deciduous teeth or damaged adult teeth). Stabilization is often not needed. Horses are sedated standing, usually with detomidine + butorphanol. A maxillary nerve block (upper jaw) or mental nerve block (lower jaw) may be performed but often isn’t necessary. Increasing amounts of direct pressure are applied to the teeth until the segment pops into position. Usually the segments are very stable when replaced. For removal, a local block may be helpful. Often the fragment is only held in place by a skin tag and the tag may be anesthetized prior to transaction or standing sedation may be sufficient.
Rostral mandibular bone fractures
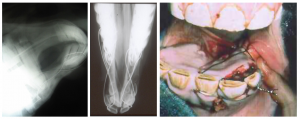
18 gauge wire is used to secure the incisors to the molars or to each other using figure 8 patterns. Repair is usually done under injectable or inhalant general anesthesia. It helps to have the horses nasally intubated rather than orally intubated if it is under inhalant anesthesia. A gag is used to keep the teeth separated. Local block of the mental nerve may be used in all ages.
Meticulous debridement permits the best reduction. Good water pressure can be obtained using a water pik or a 20cc syringe with an 18 ga needle. Curettes are useful to clean exposed bony surfaces.
Wires are passed through the bone rather than trying to fit them between the teeth. Rostral fractures may be stabilized by wiring across the incisor region (perpendicular to the fracture line is ideal). Additional wires may be necessary to prevent caudal migration of incisors. For interdental space fractures, the wires are usually secured between the first and second cheek teeth (306/307 and 406/407) and around 2-3 incisors in a woven pattern. It is possible to wire between the second and third cheek teeth if necessary. I have also wired to the bone in the interdental space for very rostral fractures or for added support.
In foals, 14 ga needles can be inserted through the soft bone to create a hole for the 18ga wire (can be passed directly through the needles). In older horses, a power drill or handchuck is useful. Drill bits or pins are chosen to be slightly larger than the wire (2mm drill bits, 1/16″ pins). Holes are drilled between teeth, avoiding the roots. If drilling is difficult, redirection should occur to avoid the likely root.
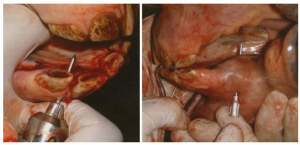
In large animals, the cheeks cannot be retracted sufficiently to allow easy placement of wire between the first two molars so access is through a small incision in the cheek. A drill guide is used to protect the soft tissues. A 14 gauge needle can be used to help guide the wire. The most common problem with direct passage of the wire is lack of penetration of the oral gingival. Oral exploration can assist. When using the needle, it needs to placed so that it can be removed without disturbing the wire (eg placed from the opposite side of the bone from which the wire is inserted).

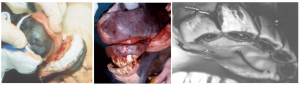
Once the wire is around the incisor teeth and the molar, twist the wire together in the interdental space. An option is to begin and end in the interdental space and twist the wire together at the end. I find this easier to tighten than when the wire is tied elsewhere. However, it is harder to protect the soft tissues from the knot. Another option is to create loops between each incisor and finish by threading the end of the wire back through the loops. Each loop is then tightened for additional stability. I have not found this degree of stability necessary in most cases. Plan on breaking at least one wire when tightening (have sufficient anesthetic capabilities to keep going). In unilateral fractures one wire may be sufficient. Most often wires are placed bilaterally.

If you are concerned about wire breakage (mouthy stallion, cribbers/windsuckers, etc) wires can be supported by dental grade methylmethacrylate. The methylmethacrylate can be used to cover the wires after placement or wires can be inserted into a methylmethacrylate brace during wire placement. A preformed brace may also be useful in comminuted fractures that tend to collapse when the wires are tightened. I have not found postoperative wire breakage to be a big concern if animals can be prevented from grazing, cribbing, etc until the bone is stronger.
Horses can survive with severe overbites or amputated lower jaws. In some instances, such as severe comminution, minimal vascular supply or nonhealing fractures, amputation may be a preferred option to repair.
Figure 8 wiring steps
– drill through bone (between teeth roots) with pin chuck or electric drill
– use 14ga needle to place wire in hole
– figure 8 around incisors and molar on ipsilateral sides
To get wire around molars, it is necessary to make an incision through the cheek
– pass needle through cheek and through hole, thread wire from lingual surface out and then back in through same hole to buccal
surface of tooth
– wire ends up on oral cavity side only, but cannot retract cheek enough to get there without making a “window” first
– finish by repeating figure 8 around incisors (alternate spaces to original) and knot with original end
– twist together the two wires in the interdental space to tighten
– cover wire ends with vinyl polysiloxane or other compound
– remove after 4-8 weeks
Tooth root involvement
The roots of teeth involved in the fracture plane are at risk due to the open nature of the fractures and immediate contamination. However, root involvement does not mandate root infection. Generally I leave the teeth in place until proven infected. Good bony union is nice before attempting repulsion or removal of problem teeth.
Vertical ramus fractures
These fractures are well covered by musculature and are usually unilateral and relatively stable due to muscle coverage. It is possible to plate these fractures if necessary. The masseter muscle is elevated subperiosteally, exposing the bone. The bone does thin in a rostral direction, potentially making implants less stable in a rostral-caudal direction.
Maxillary fractures
These fractures tend to be comminuted and open to the nasal passages. The incisive bones as well as the palate may be involved. Repair involves wiring of the affected teeth as well as wire repair of the palatal fractures, if any. Wiring to a “retainer” device or brace can help support the jaw; straight wiring can collapse the jaw in comminuted fractures. Sequestration is more of a problem and repeat evaluation should be done to remove fragments not covered by mucosa or granulation tissue.
Postoperative care
Antibiotics may be continued for 4-5 days, until granulation tissue formation can occur. Phenylbutazone is used to keep horses comfortable while eating for the first few days. If possible, the wire area should be lavaged daily to prevent erosions from impacted food. Tap water can be used but there are healing advantages to flushing with dilute chlorhexidine solution (<0.12%) or dilute doxycycline solution (inhibits collagenase and enhances reattachment of the periodontal ligament). The wires themselves will create mucosal erosions if placed tight enough to enable rapid healing. The wires should be checked daily for breakage and removed early if broken. In most cases, wires can be removed at 6-8 weeks. The erosions in the mucosa will heal rapidly.
Complications
Prognosis is generally excellent. Small fragments may sequester and require removal. This is rarely the case with mandibular fractures. Lack of blood supply to the fracture fragment is a concern in severely traumatized fractures. These usually require removal vs repair. Creation of malocclusion is possible in youngstock. This has usually been in delayed repairs in which it was not possible to fully reposition the teeth. Leaving the wires on longer resulted in a braces effect that resolved the problem.
Resources
How to perform effective equine dental nerve blocks, AAEP convention, 2004 – great pictures
Conservative Management of Unilateral Fractures of the Mandibular Rami in Horses, Vet Surg 2016, Vol.45(8), pp.1063-1065
Fracture repair techniques for the equine mandible and maxilla, EVE 2009 Vol.21(7), pp.352-357
Management of rostral mandibular fractures in the young horse, EVE 2008, Vol.20(2), pp.107-112

