Large animal cutaneous neoplasia
Sarcoids
Presentation
Sarcoids are the most common skin tumor observed in horses and are not seen in other species. While not malignant, they are very resistant to treatment and can occasionally lead to severe consequences for horses, including euthanasia or retirement.
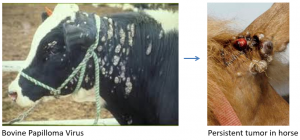
Sarcoids develop in the skin and dermal tissues due to an atypical immune reaction of horse skin to a bovine or equine papilloma virus. We assume the papilloma virus is in the horse’s skin and is “activated” by trauma. The trauma theory seems to explain the common predilection sites: scrotal area, limbs, and head as these areas are either castration sites or common sites for insect bites.
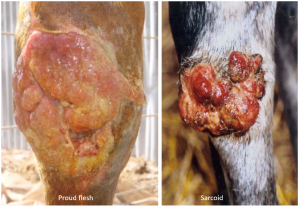
Sarcoids present in several different forms. A nodular form occurs in the dermal tissues, often with subcutaneous chains of nodules connected by bridges that may or may not be palpable. These can remain unchanged for many years and/or can start growing aggressively with trauma (including biopsy and fly bites). Some sites may be covered by normal skin; others can have ulcerated surfaces as the affected area does not heal well. Other forms of sarcoid develop an external “cauliflower” like appearance, growing into raised, often bumpy tumors of various shapes. Mixed versions are common.
Sarcoids can be grayish or can look like proud flesh (exuberant granulation tissue) and can be mistaken for such. If “proud flesh” is noted above the carpus or hock, it is most likely sarcoid or another tumor.
Sarcoids can also be flat, hairless, gray and scaly. These areas look more like ringworm or other dermal lesions rather than tumor. They are disfiguring. Many owners complain that other horse owners worry that the lesions will be contagious. Horses cannot “catch” sarcoids from other horses but it is important to rule out a true fungal disease.

Treatment
Many treatments exist for sarcoids. Whenever we have multiple treatments, it generally means nothing is 100% effective. The treatments most often used at the UMN include laser debulking (CO2 laser), cryotherapy, cisplatin beads and/or topical imiquimod. Imiquimod (Aldara®) was studied at the UMN and was found to be very effective in many sarcoids (see UMN Aldara studies). Imiquimod is a topical cream that owners can apply. It acts on toll-like receptors in the region. While we used imiquimod on its own for the study, we prefer to use it after laser therapy or with cisplatin beads, particularly in larger tumors. Combination therapy minimizes the treatment frequency and seems to optimize the results. Other treatments include electroporation (new research), radiation therapy, cisplatin or 5 -fluorouracil injections, Xxterra (blood root extract), BCG injections, autogenous vaccines, skin grafting and even topical application of fluoride toothpaste have been tried (with no evidence to demonstrate efficacy).
Surgical removal alone is not usually recommended. Most sarcoids include tendrils that grow new sarcoids as they are cut. Much like the Greek Hydra, when the main tumor is removed and these tendrils are transected, you can end up with a much bigger problem. Wide margins are a necessity and generally surgical debulking is combined with other therapies.
Sarcoids that aren’t growing, aren’t ulcerated and aren’t being traumatized should be left well enough alone. This is further supported by very recent research by Curnow et al showing that sarcoids with superficial inflammation on histology were less likely to recur. Inflammation may be protective; removing those that aren’t inflamed may result in a higher likelihood of recurrence.
As more research is done and new treatments are explored, it will be important to be able to assess study design. Most of the research on sarcoids has not been done in a controlled or blinded manner.
Not all sarcoids require treatment! If they aren’t ulcerated, raised or growing, we try not to treat. You may enter into a battle you can’t win.
Imiquimod Use
Imiquimod is a cream used in people for genital warts. It comes in small packets and prices vary widely. Imiquimod stimulates a strong local reaction without systemic effects. Imiquimod does cause reactions in normal horse skin. It can be difficult to differentiate normal reaction from flat tumor until the inflammation resolves.
- Apply 3x/week to small tumors or 1x/week to the base of tumors removed by laser or debulking. No bandage or covering is necessary.
- Clean off the concrete-like exudate prior to the next application. Soaking the area with mineral oil or warm water can help.
- Treat for 2 months. Stop treatment and re-evaluate one week later. If hair is growing back, the tumor has resolved. Restart treatment if required.
Aural plaques are another papilloma virus complication. These white plaques grow in the ears of horses and can cause ear sensitivity. Many are benign and don’t cause any issues. When they are irritating the horse, the ears can be treated with imiquimod. The amount of inflammation with treatment can be significant; the treatment works but can be challenging.

Key Takeaways
Sarcoids are the most common horse tumor and are seen in all age groups over 2.
Sarcoids develop and get angry with trauma. Plan on multimodal therapy and leave well enough alone if not growing or ulcerated.
Sarcoids grow in the dermis – NOT mucous membranes.
Resources
Management of equine sarcoids; The Veterinary Journal 291 (2023)
The Equine Sarcoid Why Are There so Many Treatment Options? VCNA Vol.35(2), pp.243-262, 2019
Efficacy of imiquimod 5% cream in the treatment of equine sarcoids: a pilot study, Vet Derm Vol.17(4), pp.259-265, 2006 (UMN study)
Histological evidence of superficial inflammation is associated with lower recurrence of equine sarcoids following surgical removal: A follow-up study of 106 tumours in 64 horses. Curnow et al. Vet J 2023 Feb.
Treatment of aural plaques and sarcoids with imiquimod
The future?
Electrochemotherapy as a single or adjuvant treatment to surgery of cutaneous sarcoid tumours in horses: a 31-case retrospective study. Vet Rec Vol.179(24), p.627, 2016
Glycolysis inhibition improves photodynamic therapy response rates for sarcoids. Vet Comp Onc Vol.15(4), pp.1543-1552, 2017
proud flesh; granulation tissue that doesn't stop when the wound is filled but continues to grow into a mound
surgical removal of as much of tumor as possible
the use of liquid nitrogen to create very cold temperatures that cause cell destruction via ice crystal formation

