Equine joint disorders
Joint anatomy and function
Development
Skeletal structures start as cartilage. Changes in the cartilage lead to ossification, bone growth, and articular cartilage formation.

If cartilage does not mature properly, the skeleton is not able to withstand normal wear and tear.
Structure
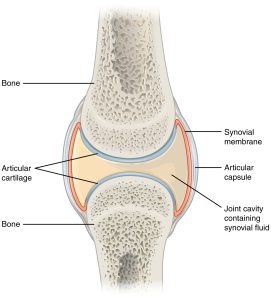
The main components of a joint include the articular cartilage (hyaline) sitting on a layer of subchondral bone, coated by synovial fluid and surrounded by a synovial lining and joint capsule. The cartilage is composed of chondrocytes and an extracellular matrix of precisely arranged type II collagen and proteoglycans. This structure traps water, creating a resilient cushion in a healthy joint. Cartilage contains no vessels, no lymphatics and no nerves. Nutrition has to migrate from the synovial fluid and through the matrix. Chondrocytes have different densities and orientation depending on the distance from the articular surface. The joint capsule maintains the joint stability (prevents motion in unintended directions) while the synovium produces lubricants, manages inflammation/phagocytosis and provides nutrition.
Extracellular matrix
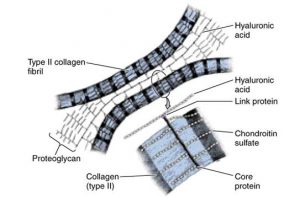
- Type II collagen – triple helix of amino acid chains, organized in fibrils. Provides tensile strength. Produced by chondrocytes. Very limited turnover of fibrils in adults.
- Aggrecan – proteoglycan; protein strand with glycosaminoglycan chains of chondroitin sulfate and keratan sulfate attached
- Aggrecans are attached to hyaluronan strands by link proteins
- The GAGs attract water creating compressive stiffness of cartilage
Synovial fluid contains nutrients and boundary lubricants. The lubricants are necessary to minimize friction between components. The main components are hyaluronate and lubricin.
Matrix metalloproteinases (MMPs) are synthesized by synoviocytes and chondrocytes. They can digest all components of the extracellular matrix and are responsible for removing damaged components. MMPs are released in zymogen form to minimize damage. Tissue inhibitors of MMPs (TIMPS) are also synthesized by the synoviocytes and chondrocytes.
Radiographic anatomy of the hock
Radiographic anatomy of the stifle

