Equine podiatry
Navicular syndrome
Navicular syndrome causes chronic forelimb lameness and is associated with pain arising from the navicular apparatus. The navicular apparatus is comprised of the distal sesamoid bone (navicular bone) and closely related structures. Multiple different clinical conditions cause pain in the navicular apparatus – these tend to look similar to each other despite different types of damage.
Navicular syndrome is most commonly identified in Quarterhorses and QH types (Paints, Appaloosas, etc). This is probably related to the pounds/square inch on their little feet. It is often bilateral.
Remember, foot pain will often cause the horse to overstress the shoulder due to changes in how the limb is advanced. This might lead owners to be more worried about the shoulder than the foot.
Pathophysiology
Function of the navicular bone
The navicular bone acts as a fulcrum to decrease the work of the deep digital flexor tendon. The fibrocartilage covered flexor surface provides a gliding surface for DDFT. Due to this interplay, the DDFT exerts a major compressive force on the distal third of the navicular bone and this force is greatest during the propulsion phase of the stride. Furthermore, the force is increased with low heel/long toe conformations. A recent study suggests navicular syndrome is a complex form of osteoarthritis (see Vet Surg, 2021 below).
See Navicular bone mechanics for useful images
Possible forms of navicular syndrome
There are multiple theories and/or possibilities on why navicular syndrome pain occurs:
- Exercise : anoxia or hypoxia causes pain with exercise
- Navicular bone pain : increased intraosseous pressure leads to bone pain
- Navicular bursa/DDFT : damage to the bursa or distal deep flexor tendon leads to adhesions and scarring in the region; pain occurs due to decreased mobility
- Coffin bone/sole/caudal hoof: other palmar heel structures are painful; this includes P3 fractures, sole bruises, and damage to other soft tissues
- Ligamentous injuries : strain/sprain of the impar ligament, collateral ligaments of coffin joint, and/or suspensory ligaments of navicular bone
- Coffin joint pain: arthritis or synovitis leading to pain on movement and with flexion
Pathological changes
Erosions of fibrocartilage of flexor surface of the navicular bone underlying the DDFT are often the first changes to occur and are typically seen on the median (sagittal) ridge. Other changes associated with the syndrome include degenerative change of the spongiosa (medullary bone), chip fracture(s) of the distal border of the navicular bone, adhesions between the flexor surface and DDFT, and navicular bursitis (rarely seen alone). Often horses have more then one of these changes by the time of diagnosis.
Diagnostics
Passive exam
Hoof testers
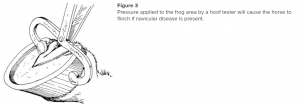
Look for pain on when hoof testers are squeezed from frog to wall and across the frog. Remember the navicular bone is deep to the frog.
Associated conformation
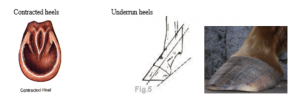
Contracted heels are often a consequence of navicular syndrome, while underrun heels and a low heel/long toe conformation can create or exacerbate the problem. You can may see a combination of contracted heels, underrun heels and long toes.
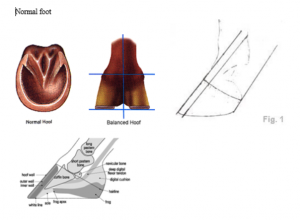
Normal conformation
Active lameness exam
Lameness examination : straight line + lunging
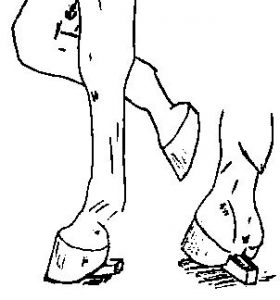
Horses with navicular syndrome usually present with a bilateral forelimb lameness. It can be difficult to see a head nod on a straight line trot since both feet hurt. The gait is described as short and choppy due to the rapid transition between sore feet. Affected horses tend to land toe first (horses should normally land flat footed or slightly heel first). They also tend to stumble more. Lameness is accentuated by turning the horse on a hard surface and in a tight circle (lunging). With lunging, the inside leg is typically more lame and the lameness switches between feet depending upon the direction lunged.
Distal limb flexion : if this test is positive, look for coffin joint pain/ligamentous pain/navicular bone pain. Major sources of coffin joint pain include a broken forward hoof axis (mild club foot) and medial-lateral hoof imbalance. If you don’t see those, the flexion response may be due to increased pressure within the navicular bone.

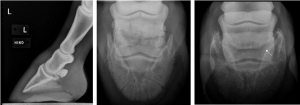
Wedge tests
- Frog wedge : To do this test, a board or hoof knife is placed under the frog and the horse made to stand on it for 1 minute by lifting the other foot. Consider this test a hoof tester using the horse’s entire body. If this is positive, look for pain in the navicular bone or caudal P3.
 Tracy Turner, DVM
Tracy Turner, DVM
- Toe wedge : To do this test, a board or hoof knife is placed under the toe at the front and the horse made to stand on it for 1 minute by lifting the other foot. This places stress on the deep digital flexor tendon. If this test is positive, look for pain in the navicular bursa, flexor cortex of the navicular bone or flexor tendons.
Circulation test : After 15 minutes of exercise, horses should increase the skin temperature in the heel region by at least 1°F. If they do not, this may indicate poor blood flow to the heel region. This test is subject to outside influences : do not jog the horse prior to doing the test and it may be inaccurate on very cold and very hot days.
Local blocks
Coffin joint block: typically blocks the coffin joint, collateral ligaments of the coffin joint, navicular bursa and navicular bone pain. With enough local anesthetic (>6cc) and time (>5 min), this block also blocks the sole and heel region as the local anesthetic diffuses out of the joint.
Bursal block : blocks the bursa and the heel regions. This is a very low PDN block; it usually numbs the navicular bone but should not numb the coffin joint
Palmar digital nerve block (PDN): blocks the navicular bone, coffin joint, bursa, caudal heel region and sole (all of the foot except for the dorsal laminae and the coronary band)
| Test responses | Bursa positive (improves) | Bursa negative |
| Coffin joint positive | bursa, navicular bone, sole, navicular ligaments/ tendons/heel | coffin joint and coffin joint collateral ligaments |
| Coffin joint negative | (navicular bone), navicular ligaments /tendons/heel, P3 | navicular ligaments /tendons/heel, P3 |
Imaging
MRI is the gold standard. Scintigraphy can also help localize lesions within the foot.
*Radiographic changes are not pathognomonic for navicular syndrome (false positive and false negative results can occur)*. However, radiographs can be performed in the field and are often part of a “prepurchase” exam.
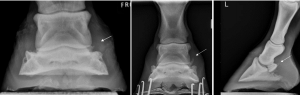
Standard radiographic views
Lateral view – use to check hoof pastern axis, signs of laminitis, toe length, heel angle, soft tissue swelling, fractures, arthritis, shape of navicular bone, sole angle (angle between the ground and bottom of P3), sole shape (flat /cupped)

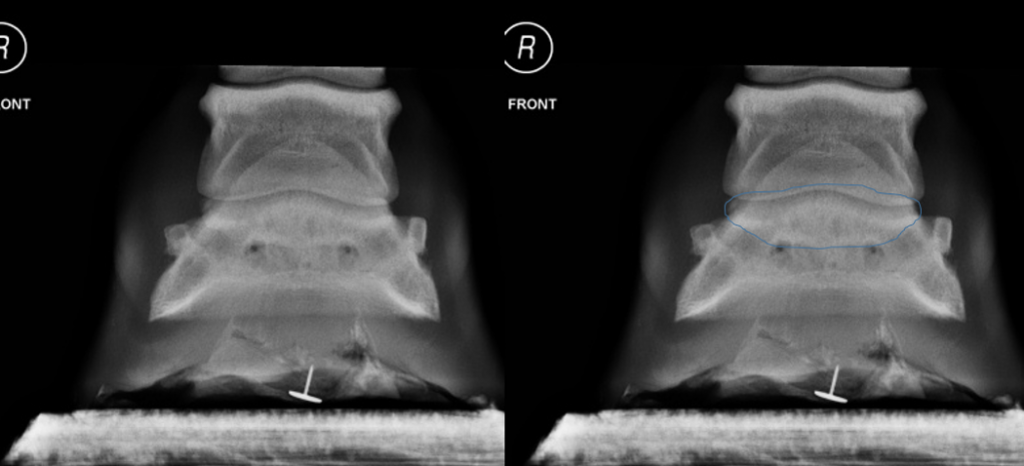
Dorsopalmar view – use to check for medial-lateral imbalance, soft tissue swelling, fractures, arthritis, navicular bone remodeling (wings)
P3 view (60 degree) – use to look for navicular bone fractures, bone asymmetry, cysts, synovial invaginations, and remodeling

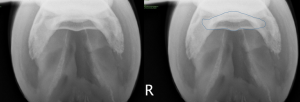
Flexor cortex view- use to evaluate shape of navicular bone, assess for medullary sclerosis
Radiographic changes consistent with navicular syndrome
- Remodeling of the wings and dorsal surface of the navicular bone
- evident on dorsopalmar, P3, and lateral views
- remodeling may appear as sawtooth borders of the navicular bone, a bump on dorsal surface, and/or spurs on the extremities of the bone
- Synovial invaginations
- evident on P3 view
- navicular bone is considered abnormal if many “lollipops” (invaginations shaped like lollipops) are evident on the base of the navicular bone or if lollipops are present on the sides of the bone
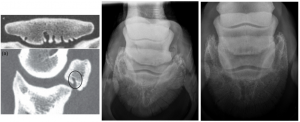
3. Bone cysts
- evident on flexor cortex view, lateral view
- hole in middle of navicular bone

- Flexor cortex changes
- evident on flexor cortex view
- abnormalities include flattening of flexor cortex, sclerosis of navicular bone and/or lysis of cortical surface
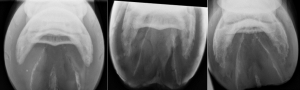
- Navicular bone fractures
- evident on dorsopalmar view, pedal view
- includes chips or complete fractures
Contrast study : performed to assess cartilage on flexor cortex

Remember to check for other issues:
- medial-lateral hoof balance
- pastern-coffin bone axis (broken back or broken forward)
- heel angle (underrun?)
- toe length/foot balance
- evidence of previous laminitis
- arthritis
- pedal osteitis (increased irregularity to border)
Treatment
- Treat specific lesions – e.g. DDFT tear found in MRI
- Corrective shoeing
- Encourage horse to land normally rather than on toe
– Correct long toe, underrun heel - Raise the heel to decrease strain on DDFT and forces on navicular bone
- Roll the toe to ease breakover
- Egg bar shoe to provide support to heel area
- Encourage horse to land normally rather than on toe
- Medical management
• Systemic NSAIDS
• Intrasynovial corticosteroids (triamcinolone)
– Distal interphalangeal joint
– Navicular bursa (tends to be the most effective)
• Bisphosphonates – alter bone metabolism by interfering with osteoclasts – controversial - Keep the horse in regular work
- Surgical management
• Transection of the proximal suspensory ligament of the navicular bone
– can be done arthroscopically
– effects are likely due to transection of sensory nerves to the navicular bone
• Palmar digital neurectomy
– Last resort but can be helpful
– Fraught with complications (e.g., neuroma formation, DDFT rupture)
Typically, both the medial and lateral PD nerves are transected on each foot. After neurectomy, the foot will be desensitized and needs protection because they will not notice trauma. This usually means horses are kept in a pad + shoe. The horses are NOT more prone to stumbling and will usually stumble less since they land properly (not toe first). Eventually nerve sensation will regrow.
The neurectomy will NOT improve lameness more than a PDN block does. Do the block first. If it doesn’t make much difference in horse comfort, neither will the neurectomy.
Key Takeaways
Horses with navicular syndrome are often QH types, typically bilaterally lame and present with a short choppy gait. The lameness is worse when circled and they respond to a palmar digital nerve block.
Navicular syndrome does NOT necessarily mean the navicular bone is diseased. It is a very complex disorder.
Treatment is generally to fix the foot conformation (farrier work), keep the horse in work and comfortable (joint injections and NSAIDs). Palmar digital neurectomy is considered when that no longer works.
Supplemental
Resources
The equine navicular apparatus as a premier enthesis organ: Functional implications. Veterinary Surgery. 2021;50:713–728.
Current concepts of navicular disease, 2011 EVE
Influence of trimming, hoof angle and shoeing on breakover duration in sound horses examined with hoof-mounted inertial sensors, Vet Rec 2021 – good explanation of breakover and how shoes impact it
2000 What is your diagnosis JAVMA 216(9): 1393-1394 -navicular bone fracture
Other Clinical Problems of the Equine Foot Vet Clin Equine 37 (2021) 695–721
Used in horses to describe the end of the stance phase: the period of time from when the heel is off the ground to the time when the toe is off the ground. This time window is prolonged with long toes and when a horse is shod. A longer breakover requires more joint motion.

