2.0 Introduction
The Mystery of HIV Resistance
Acquired Immune Deficiency Syndrome (or AIDS) refers to a suite of symptoms associated with Human Immunodeficiency Virus (or HIV). Untreated individuals infected with HIV have a compromised immune system and are unable to combat common infectious agents. Basically, the virus enters the t-cells of the human immune system and commandeers these cells for its own purposes. Thus, the immune system is re-purposed to make more HIV, rather than fight infections. Without treatment, people with AIDS often suffer and die from the combined effects of several common pathogens—e.g., pneumonia, tuberculosis.
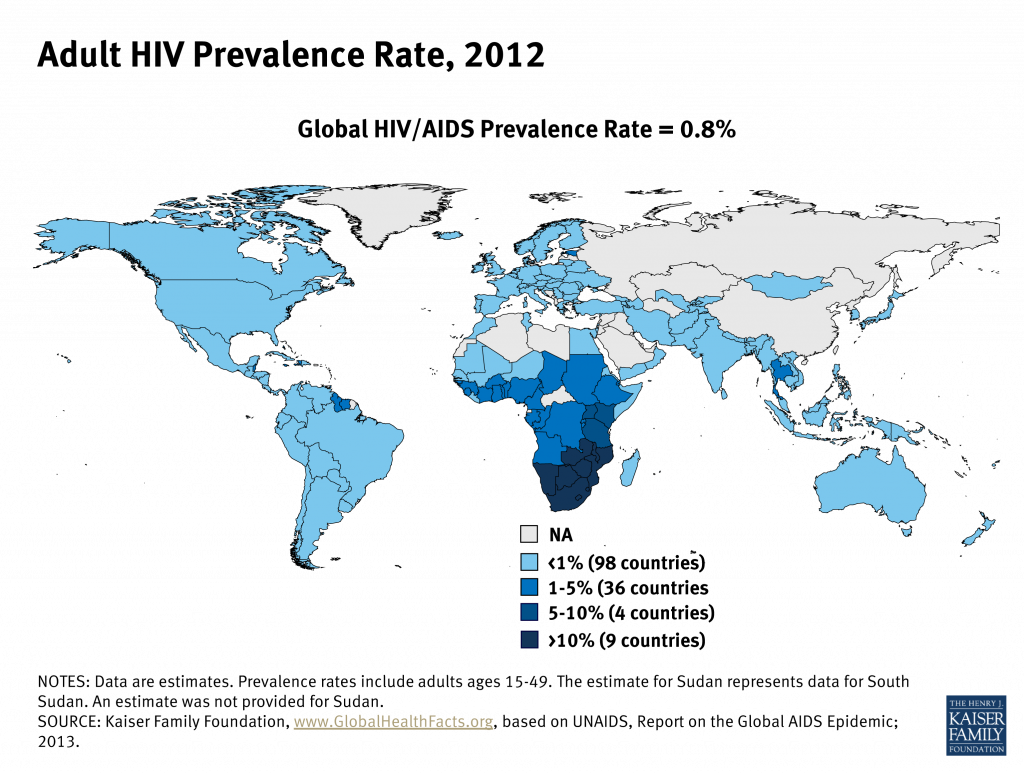
The impact of HIV infection is devastating: approximately 30 million people have died from AIDS-related causes, and at least that many are currently living with AIDS. In 2010 alone, 1.2 million adults and children died from AIDS in sub-Saharan Africa. And today, nearly 20 million children have lost their parents to AIDS.
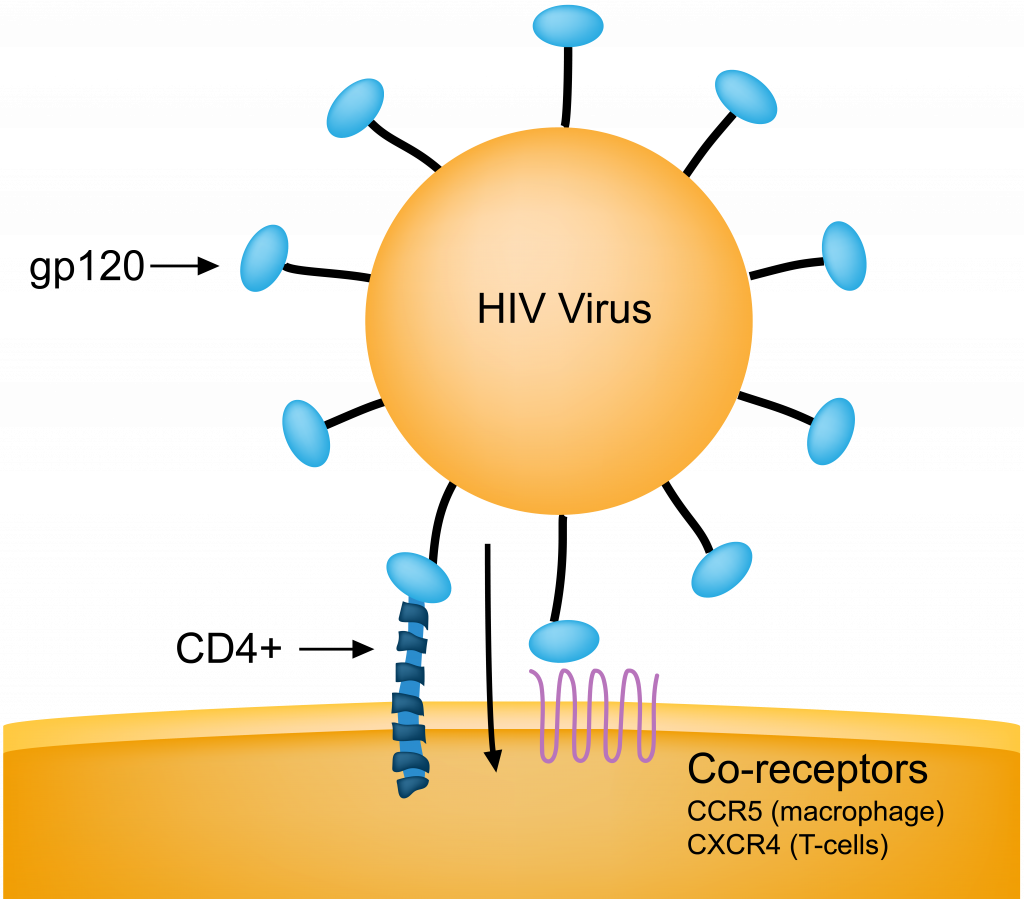
Understandably, the discovery that some people are resistant to HIV infection was met with considerable enthusiasm. Follow-up work revealed that resistant individuals have a genetic variant, or allele, for a specific gene—CCR5. This gene codes for a cell-membrane protein, also called CCR5, which typically facilitates the incorporation of HIV particles into host immune cells (see Figure 1). Resistance to HIV is associated with one or two copies of a defunct version of the CCR5 gene. Being born with a copy of the non-functioning version of CCR5 is clearly desirable, given the death toll associated with HIV infection and AIDS.
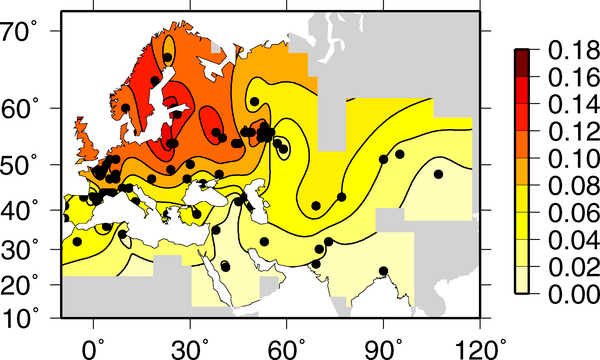
But there’s a catch: the advantageous CCR5 gene is most common in Europe, especially in Northern Europe. For example, approximately 25% of Icelanders sampled had a non-functioning (and therefore desirable) version of the gene. In Britain, Spain, and Italy, the frequency of the resistant allele is 11%, 9%, and 5%, respectively. Yet in Nigeria, with over 3 million people living with AIDS, only 1 of 111 people sampled had a copy of the resistant allele. And in Kenya, where almost 7% of the population is infected with HIV, the resistant allele has not been detected.
Points to Ponder
- How is it possible that resistance is most common where it is least necessary?
- Why aren’t there more resistant individuals in Sub-Saharan Africa, where the death toll is so great?
- Finally, can an understanding of evolution help us understand these harsh realities?

