13.8 Female reproductive physiology
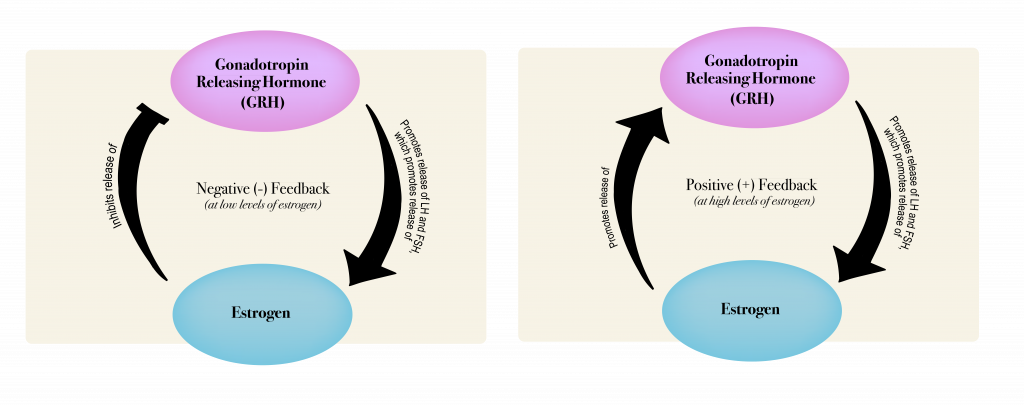
Female reproductive anatomy and physiology has many similarities to that of the male. As described earlier, females also use LH and FSH secretion from the pituitary triggered by GRH from the hypothalamus to stimulate hormone production by the gonads. There is also negative feedback to regulate hormone production. However, in females, the interplay among the hormonal signals is more complicated than in males. While male hormonal feedbacks and signaling provide a relatively steady level of the sex hormone testosterone, for females there is a monthly cycle over which the circulating hormone levels go up and down at the same time as changes occur in the ovaries and the uterus. This surging of hormones along with the changes in the ovaries and uterus require the more complicated physiological controls described below.
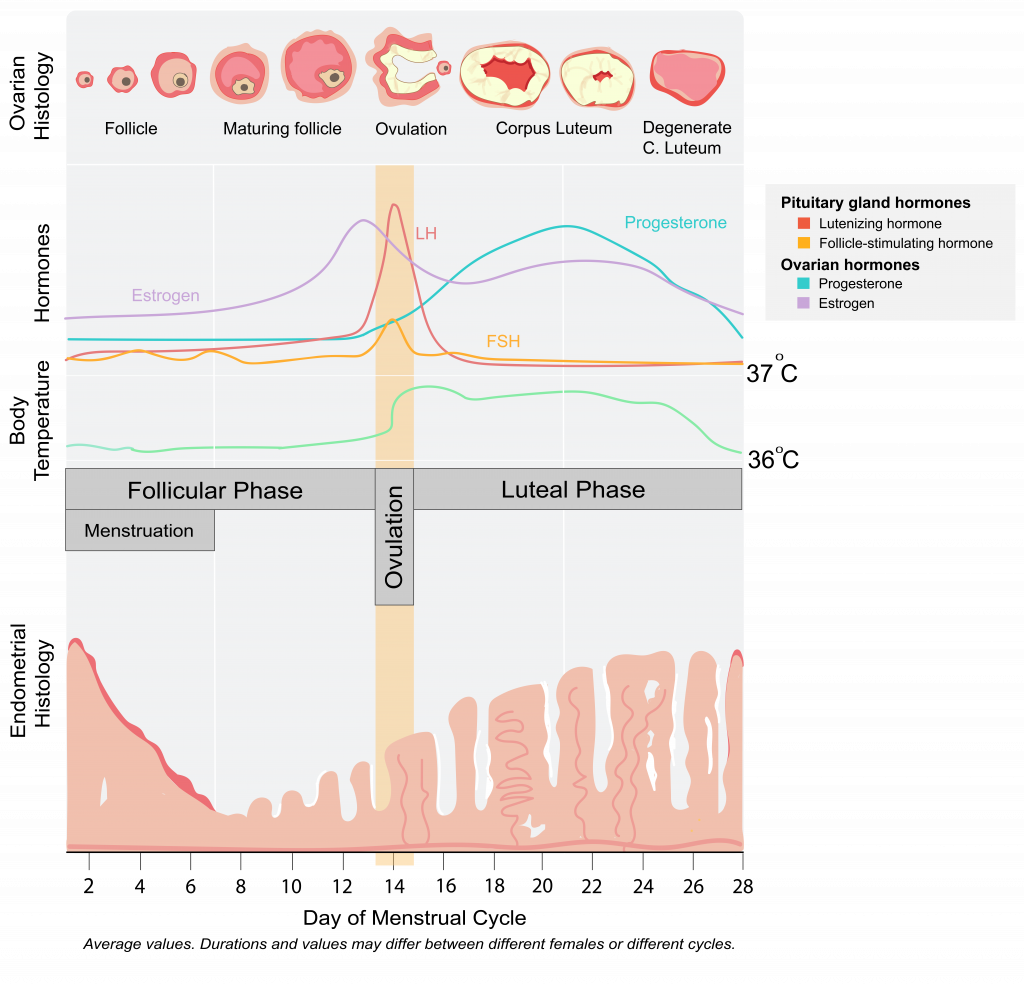
The monthly female reproductive cycle can be divided into three phases, the follicular phase, ovulation, and the luteal phase. For each of these phases, there are concurrent changes happening in the uterus and in the ovaries. See the figure below for a diagram of the phases of the female reproductive cycle and what is happening in the ovary, the uterus, and circulating hormone levels.
The Follicular Phase
The name “follicular phase” is in reference to the egg-containing follicle in the ovary that matures during this phase (note the ovarian histology shown in Figure 7). This phase begins on day one of a female’s reproductive cycle. Day one is defined as the first day of menstruation (the first day of a period). Menstruation occurs for about the first 5 days of the follicular phase. During these days, if a female is not pregnant, low circulating levels of the hormone progesterone trigger the breakdown of the endometrium (the lining of the uterus). This blood-rich tissue exits the uterus through the cervix and then leaves the body out the vagina. During menstruation, low circulating levels of estrogen and progesterone stimulate GRH production (from the hypothalamus in the brain), which leads to LH and FSH secretion by the pituitary gland. FSH signals the maturation of several follicles within the ovaries. These follicle cells produce a steadily increasing amount of estrogen (note the estradiol (a type of estrogen) increases from day 1-12 in Figure 13.7). In the early follicular phase, the estrogen provides negative feedback for LH and FSH production. About 5 days into the follicular phase, after menstruation is done, estrogen production causes the endometrial layer of the uterus to begin to thicken, preparing the uterus for a fertilized egg. While several follicles in the ovary begin the maturation process, most times only one follicle in one ovary becomes dominant and continues to mature. At around the 12th day of the follicular phase, estrogen levels reach a high enough level to trigger a switch from estrogen providing negative feedback on GRH and therefore LH and FSH secretion by the pituitary, to estrogen providing a positive feedback (diagrammed in Figure 8). At this point the estrogen triggers increased GRH release, causing more LH and FSH release, causing a spike in circulating LH and FSH levels (note the LH and FSH spike between day 12 and 15). The spike in these hormones causes ovulation.
Check Yourself
Ovulation
Ovulation refers to the rupture of a mature follicle within the ovary; this ruptured follicle releases an oocyte (an unfertilized egg) into the abdominal space. Because this rupture is an actual breakage, some females will feel a twinge or slight pain during ovulation. Ovulation generally happens around day 14 of the reproductive cycle in one ovary. The oocyte travels into the oviducts and there completes meiosis I, yielding an oocyte and a smaller polar body. (Meiosis I begins when a female fetus is in utero, and it pauses for years until that female fetus is born, develops, and begins ovulation). At ovulation the oocyte begins meiosis II, but will only complete meiosis II if the oocyte is fertilized.
Luteal phase
During the luteal phase, the now empty follicle within the ovary collapses. This collapsed mass of cells is called a corpus luteum. The corpus luteum produces progesterone that enters the blood circulation. Progesterone signals the hypothalamus to signal the pituitary to reduce FSH and LH production, which prevents other follicles from maturing. If the oocyte in the oviduct is not fertilized, the corpus luteum degrades, causing a drop in progesterone, which triggers the beginning of menstruation and the return to the follicular phase of the reproductive cycle (back to day 1 after about a 28-day cycle).
If the oocyte is fertilized by a sperm in the oviduct, the oocyte completes meiosis II, forming a fertilized egg (now called a zygote) and another polar body. The zygote travels through the oviduct, going through several cell divisions until it is called a blastocyst. Then, the blastocyst implants into the uterine lining. At this point the blastocyst begins producing the hormone human chorionic gonadotropin (HCG), which signals the corpus luteum in the ovary to continue to produce progesterone. (HCG is the hormone detected by home pregnancy tests.) This continued elevated progesterone in the blood prevents the shedding of the uterine lining so that a pregnancy can be maintained. Eventually, after about 12 weeks of embryonic development, the placenta (the organ that connects the developing fetus to the mother) takes over the production of progesterone and the corpus luteum degrades. At this point, the embryo is referred to as a fetus, and will continue fetal development assisted by the placenta.

