3 Liver function testing
With liver dysfunction, problems can arise with coagulation, protein levels, energy levels, and toxins.
Liver damage can be assessed through analysis of liver enzymes and products as well as by liver function “tests”. We look for loss of cellular contents, changes in liver function and signs of liver dysfunction.
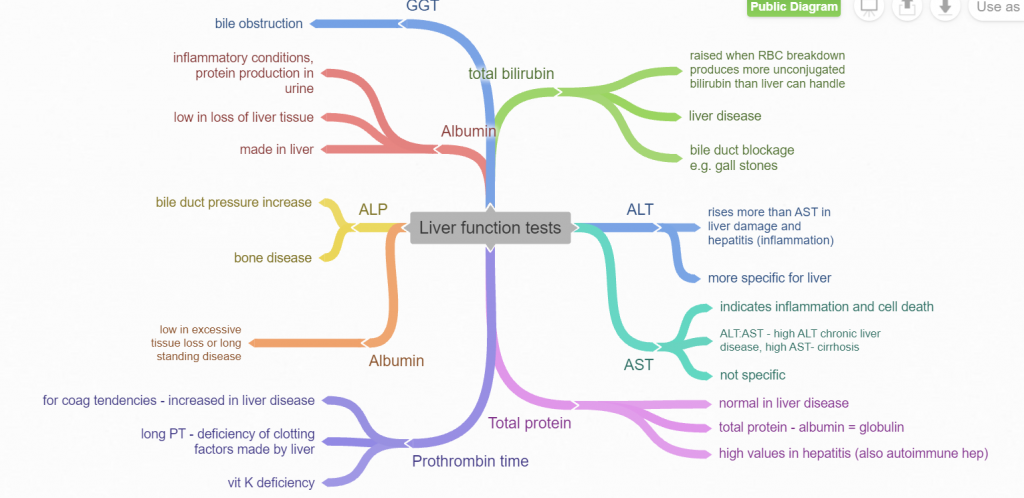
SERUM MARKERS
Leakage enzymes = hepatocellular damage
AST* and ALT will be elevated with hepatocyte damage, while ALP and GGT are more typically elevated with bile stasis or bile duct pressure.
AST, ALT, LDH, and SDH (transaminases) exist within the hepatocytes and are released into the blood stream when the hepatocytes are damaged.
In dogs and cats, ALT is the most useful as it is much more liver specific. However, it can be released from muscle cells too so doesn’t necessarily indicate liver damage.
Horses and ruminants have low levels of ALT in hepatocytes so it isn’t very useful. SDH is much more useful in those species.
AST is also released from muscle cells in all species but be used to identify hepatocyte damage if muscle enzymes are low.
GDH (GLDH) is used in other countries but is not routinely available in the US.
All leakage enzymes values may also be normal in end stage (cirrhotic or scarred) liver disease as the cells have already released theses factors.
From this video
Induced enzymes = biliary stasis
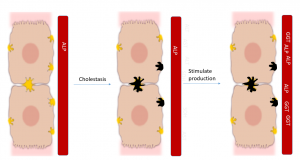
ALP and GGT are produced with biliary stasis. Liver levels are normally low when everything is working well. ALP is also produced in bone, kidney and placenta and is further stimulated by corticosteroids. ALP levels are normally elevated in young growing animals.
GGT is considered to be an induced enzyme but can be released with acute hepatocellular damage. Many other cell types also produce GGT, especially the pancreas and the kidney. However, the kidney and pancreas elevations do not usually result in increased serum levels of GGT.
GGT is considered more specific but less sensitive than ALP for liver damage in dogs. This means you can have liver damage and normal GGT levels, but if you see GGT levels, you can be pretty sure you have liver damage. In cats, GGT is more sensitive but less specific. GGT will go up with mild liver damage but other things can cause elevations. Generally we perform both tests in small animal species.
In large animal species, just GGT is used in most cases. Keep in mind that other things can lead to increases in GGT (not just the liver).
LIVER FUNCTION TESTS
More specific liver function evaluation includes measuring prothrombin (clotting function), albumin, and bile acid levels.
Serum bile acids
Bile containing bile salts is released into the duodenum in response to elevated cholecystokinin (CCK) and secretin levels. Secretin is released when the pH in the duodenum is lowered (more gastric contents). Secretin stimulates biliary cells to produce bicarbonate and water, expanding the volume of bile and increasing biliary flow. CCK is released when fat-containing chyme is present in the duodenum and it stimulates gall bladder contraction and biliary flow.
The released bile aids in fat emulsification and absorption. Some of the bile salts are reabsorbed passively in the proximal intestine but most are actively transported back into the blood in the ileum. 90-95% of the salts are returned to the liver. In the liver, the bile salts are extracted and reused. This process repeats 10-12x per day, creating the enterohepatic cycle. Small amounts of bile salts escape absorption and pass into the colon where they are broken down by bacteria. These products create the brown stool color and yellow urine color.
Increased serum bile acids occur with
- abnormalities in the portal circulation – congenital or acquired vascular shunts move blood away from the liver, preventing the first pass metabolism and impeding removal of bile acids from the circulation. Bile acids stay in the systemic circulation
- decreased functional hepatic mass – diffuse liver disease results in impaired uptake of bile salts from the portal vein
- decreased bile acid secretion in bile – any cause of cholestasis can lead to back pressure and move bile acids back into the circulation
Bile acids are very sensitive indicators of cholestasis and liver damage. Any jaundiced patient will have elevated serum bile acids but they can be useful in determining the cause of the jaundice and help with identifying diffuse liver damage. Generally bile acids are measured both before and after eating in dogs and cats; a single sample is adequate in herbivores.
Increases in fecal bile acids are indicative of malabsorption, which can cause diarrhea. However, our ability to accurately assay fecal bile acids is currently questionable.
Plasma ammonium levels
Ammonia is produced by intestinal microbes, reabsorbed into the blood and removed by the liver. The liver uses the ammonia for urea and protein synthesis. Ammonium levels are elevated with changes in hepatic blood flow and decreased functional hepatic mass. Levels can be elevated by strenuous exercise, urea toxicity and other conditions but not with cholestasis. This means ammonia levels provides a nice comparison to bile acid levels. Ammonia measurement is not a very sensitive test but is useful to measure in cases of suspected hepatic encephalopathy.
Other liver products
Albumin is produced by the liver. Hypoalbuminemia (low albumin levels) is quite common in dogs with loss of 60-80% of liver function. It is not as commonly seen in horses.
Globulins are also produced by the liver but may be elevated in liver disease. Elevations in liver disease are likely due to less processing of foreign compounds by the hepatic Kupffer cells, resulting in an increased immune response.
Glucose levels may be either decreased, increased or normal, depending on other mechanisms involved.
Urea is produced in the liver and may be decreased with liver disease; however, urea can be decreased for many reasons unrelated to liver disease.
Cholesterol is produced in the liver. Levels may be low, normal or elevated and depend in part on if cholestasis is a component of the liver dysfunction.
Clotting factors are produced in the liver. Liver dysfunction can lead to coagulopathies and prolonged bleeding times due to low levels of clotting factors.
CLINICAL SIGNS
Loss of liver function can lead to clinical signs, including
- pruritis due to accumulation of bile salts in the skin
- pale smelly fatty feces due to loss of fat absorption
- petechiation, brusing and/or bleeding due to limited production of coagulation proteins and/or storage of vitamin K
- hepatic encephalopathy (neurological signs) due to accumulation of toxic products and limited urea cycle activity
- seizures due to changes in glucose regulation
- see youtube video
- poor growth due to limited nutrient storage
- icterus or jaundice due to bilirubinemia
- edema or ascites due to changes in colloid oncotic pressure
Key Takeaways
| Test | Indicates |
|---|---|
| AST/ALT/SDH elevated | hepatocellular damage |
| ALP/GGT elevated | biliary stasis or damage |
| Serum bile acids elevated | liver damage |
| Albumin low | liver failure |
| Prothrombin (bleeding) times prolonged | liver failure |
| Ammonia elevated | liver failure |
Pattern recognition is important
| Hepatocellular damage (liver parenchymal damage) | Cholestasis (gall bladder/bile duct damage) | |||||
|---|---|---|---|---|---|---|
| ALT/AST/SDH | GGT/ALP | serum bile acids | ALT/AST/SDH | GGT/ALP | serum bile acids | |
| increased | normal | high | normal | increased | high | |
End stage liver disease may be accompanied by normal AST/ALT as all cells have released their contents. Diagnosis may be via low albumin, high ammonia, prolonged bleeding times, and high serum bile acids.
ALT = alanine aminotransferase
ALP = alkaline phosphatase
AST = aspartate aminotransferase
GDH = glutamate dehydrogenase
GGT = gamma glutamyltransferase
SDH = sorbital dehydrogenase
Resources
Liver enzymes; UGA free ibook
Ingesta mixed with salivary and gastric juices
The process by which something excreted in the bile into the intestinal tract is reabsorbed and returned to the liver. Common components are bile acids and drugs.
abnormal behavior and brain function related to liver dysfunction and high levels of ammonia
itchiness
Swelling caused by accumulation of fluid in the tissues
accumulation of fluid in the peritoneal (abdominal) cavity

