17 Pancreatitis
Preventing pancreatitis
The pancreas has high self destructive capacity. It contains enzymes that destroy protein and lipids. It is comprised of cells that have walls of protein and lipids.
Zymogens are activated by:
- Calcium
- helps trypsin activation
- Proteases
- released from lysosomal granules
- Trypsin
- activates other enzymes
To prevent self digestion, several safety mechanisms are built in:
- Low calcium levels stabilize trypsinogen
- keep it from changing into trypsin
- Trypsin inhibitors are also present in the pancreatic cell
- SPINK – serine protease inhibitor
- these bind active trypsin and keep it from working
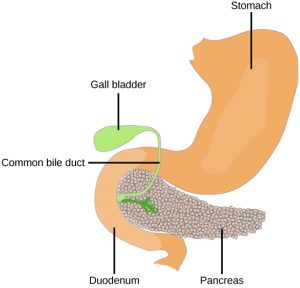
- CFTR secretes sodium bicarbonate and flushes the duct system
- Move activated products into the duodenum
- Sphincter muscle at end of duct next to duodenum
- keep calcium, lysosomes and endopeptidases out of the pancreas
Failure of the safety mechanisms leads to inflammation of the pancreas = pancreatitis
Potential activators
- Idiopathic
- we don’t know
- Ingestion of fatty foods
- this probably leads to excessive release of CCK
- more CCK means more trypsin; both can flow up the pancreatic duct
- Endocrine disorders
- diabetes and pancreatitis are closely linked
- which comes first?
- Inflammation
- inflammation means more cells with lysosomal granules
- inflammatory cells can flow up and down the ducts, activating things
- this is worse in cats due to the combined bile duct and pancreatic duct
- pancreatic duct blockage
- parasites, inflammatory cells, tumors can block the duct
- this prevents the natural sodium bicarbonate flush mechanisms
- activated trypsin stays in the pancreas vs being flushed out
- medications
- several drugs can activate trypsin
- particularly a concern in animals being treated with cancer chemotherapy
- ischemia- reperfusion injury
- ischemia – loss of blood flow; reperfusion – return of oxygen
- I-R leads to free radical formation
- free radicals can activate lysosomal enzymes
- this likely occurs with gastric dilatation volvulus in dogs
- blunt force trauma
- trauma can cause release of lysosomal enzymes
- hit by car
- surgery – it is easy to damage the pancreas
- genetic disorders
- CFTR gene
- SPINK gene
- we know some breeds (terriers, Siamese) are more prone to pancreatitis
- research area
- hypercalcemia
- high serum levels of calcium will lead to higher levels of calcium in the pancreas
- hypercalcemia is seen in older cats with hyperthyroidism and in animals with paraneoplastic syndromes
Pathophysiology
When enzymes are activated in the pancreas, they do start digesting the pancreas itself and the intrinsic vessels. The melting pancreas can cause severe peritonitis (inflammation of the abdominal cavity) and/or become infected. Enzymes eventually leak into the bloodstream and get disseminated to the body. While the gut is designed to “control” the enzyme action, this isn’t true in the kidney and other areas of the body. Digestion in other areas leads to inflammation and hemorrhage.
Abscesses, cysts and shock develop. Organ failure can follow (particularly renal failure). Many animals go into disseminated intravascular coagulation (DIC = death is coming). As multiple clots form throughout the body, all the clotting factors are used up and the animals start spontaneously bleeding.
Acute pancreatitis
Clinical signs in dogs
- unnoticed
- vomiting
- diarrhea
- abdominal pain
- shock
- hemorrhage, ecchymoses, petechiation (all forms of bleeding)
- death
Vomit and die syndrome – due to vagal nerve stimulation by the pancreatic inflammation, vomiting can lead to cardiac asystole (heart stops).
Many causes of vomiting and diarrhea are not directly related to the GI tract. Pancreatitis is one of the important ones to consider as it can be life threatening and often needs aggressive treatment. Dogs typically exhibit abdominal pain, vomiting, dehydration and death.
Clinical signs in cats
- unnoticed
- lethargy
- dehydration
- polyuria/polydipsia (drink more, pee more)
- poor appetite
- vomiting
- weight loss
Cats tend to get triaditis – inflammation of the duodenum, biliary system and pancreas. Cats show very vague signs and don’t usually die. Cats show mostly lethargy and anorexia, followed by dehydration and jaundice. Vomiting and diarrhea are rare in cats. Many will develop chronic pancreatitis.
Treatment
Both dogs and cats are treated for pain, gastric ulcers, infections, and for dietary deficiencies (vitamin B12 is often required). While going NPO (nothing per os) rests the pancreas, it can have severe consequences of its own, particularly in cats. Dogs are fed a bland diet and cats fed a bland, high calorie diet. As cats are often anorexic, a feeding tube is often required. Fluids and colloids are given as needed.
Chronic pancreatitis
Chronic pancreatitis is probably an under-diagnosed condition. Animals may be subclinical (not showing signs) but still develop fibrosis (scarring) and atrophy of the pancreas. This means the pancreas cannot return to normal status. However, the pancreas can function normally with only 10% normal tissue.
Affected animals will show similar signs to acute pancreatitis but are not usually at risk of dying unless they get a form of acute pancreatitis on top of their chronic pancreatitis. Abdominal pain can be helpful in differentiating vomiting or diarrhea related to pancreatitis from other causes.
Animals with chronic pancreatitis should be managed to minimize risk factors for pancreatitis. Maintaining a healthy weight is important. Most dogs need to be put on a low fat diet, eating mostly lean proteins and carbohydrates. Cats should stay on food, even if it means using a feeding tube.
Chronic pancreatitis can lead to diabetes mellitus and exocrine pancreatic insufficiency.
Resources
New insights into the etiology, risk factors, and pathogenesis of pancreatitis in dogs: Potential impacts on clinical practice, J Vet Intern Med. 2022;36:847–864.- accessible review
Pancreatitis in dogs – client focused
SPINK gene and pancreatitis – research article
Feline triaditis – vet article

