37 Regurgitation
Regurgitation is the release of food back out of the mouth when the food has not reached the stomach (undigested). It is usually related to esophageal dysfunction or obstruction.
Pathophysiology
Esophageal disorders lead to regurgitation or retrograde flow of the bolus back up and out the mouth. Most disorders are related to poor muscle tone or neurogenic disorders affecting the esophagus.
Physical obstructions can occur with food, treats and toys or with esophageal strictures. Strictures are relatively common after esophageal trauma (eg after choke in horses). Occasionally congenital anomalies (eg persistent right aortic arch) entrap the esophagus, creating a physical obstruction.
Idiopathic (unknown cause) megaesophagus is the most common cause of regurgitation in dogs 7-15 years of age. Congenital megaesophagus and myasthenia gravis can cause similar signs as can several other endocrine disorders.
Diagnostics
Watching the animal is important to differentiate between regurgitation and vomiting. Depending upon the history, further testing may be important to differentiate physical obstruction from functional obstruction.
| Regurgitation | Vomiting |
| Passive | Active-heaving |
| Minimal warning | Owners hear retching |
| Owners don’t hear it | Prodromal phase – nausea (lip licking, salivation) |
| Food undigested | Digested food |
| Tubular in shape | Bile staining possible |
Food, treats and toys causing physical obstruction can be visualized with radiographs (SA) and endoscopy (LA).
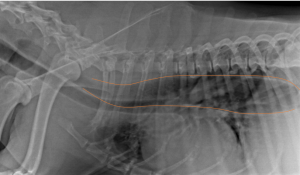
The esophagus is not generally radiographically visible in normal animals.

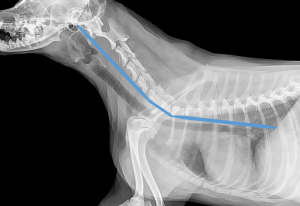
Animals with esophageal dysfunction may have swallowed air present in the esophagus.
Contrast studies using regular films or fluoroscopy can help identify megaesphagus and motility disorders. Food is mixed with barium to be able to follow the food during imaging.
Megaesophagus films

Endoscopy is very useful in horses since they can be scoped while standing and awake.
Choked horse clinical signs
Dogs with regurgitation without a diagnosis should be tested for myasthenia gravis (test for anti-acetylcholine receptor antibodies), for thymoma via thoracic radiographs, Addison’s disease via ACTH stimulation test, hypothyroidism via a thyroid panel (T4, FT4, TSH) and for lead toxicity.
Therapy
Many esophageal obstructions can be removed endoscopically. Myasthenia gravis is treated with anticholinesterase inhibitors. Immune or inflammatory conditions can be treated with systemic or local steroids. Vitamin E and thyroid supplements are given for for related deficiencies.
Most other disorders, including megaesophagus, are treated symptomatically. Symptomatic treatment may include changing the consistency of food (creating a slurry or a meatball), elevated feeding and/or treatment with proton pump inhibitors and sucralfate (ulcer therapy).
Key Takeaways
| Dysphagia | Regurgitation | |
| Eating trial | Watch to see if can chew and swallow | Watch to see if stuff comes up and if abdominal effort |
| Oral exam | Check for dental issues, oral sores and oral foreign bodies | |
| Radiographs (plain) | Check for dental issues, foreign bodies and masses | Check for foreign bodies and masses |
| Radiographs (contrast) | Check for air in the esophagus | Check for normal bolus movement |
| Endoscopy | Check teeth and pharynx | Check for foreign bodies, masses and activity |
| Fluoroscopy | Evaluate swallowing | Check for normal bolus movement |
Just for fun
How does my stomach work – good explanation of esophageal reflux disease and hiatal anatomy
Vascular ring anomalies in dogs and cats, UGA free ibook
Vomiting cat – Shrek
How bird vomit helps us understand history – really bird regurgitation
Unchoking a horse the old fashioned way – sedatives are more commonly used now to relieve the choke with less irritation and risk

