9 Leptospirosis
Leptospirosis
Author: Bradley Fountain
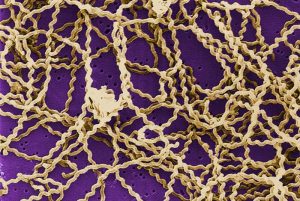
Leptospira interrogans, the most common and persistent pathogen species responsible for the disease leptospirosis, is a Gram negative spirochete endemic to most of the world, especially in areas with standing water or seasonal floods. The species contains over 200 known pathogenic serovars and is very zoonotic, transmittable between different animal species and to humans with no significant barriers. The bacteria are shed through the urine. Animals are infected by drinking contaminated water and humans through mucosa or broken skin exposed to the same. The bacteria then travel through the blood and multiply in a variety of organs, causing tissue damage through a mechanism likely related to the organism’s lipopolysaccharide coating. The immune system is largely capable of clearing the bacteria from the body except in the kidney tubules, where the bacteria persists and continues to multiply, being shed once more in urine.

As a disease, leptospirosis is only partially understood. In humans, the bacteremia caused by initial infection brings on flu-like symptoms. This is followed by a brief period of pseudo-latency when the bacteria are sequestered in organs and begin multiplying, after which signs of disease re-emerge due to related tissue damage. In domestic animals the bacteremic stage can be difficult to detect, as symptoms can be as general as mild malaise or lethargy and moderate fever. If a veterinarian is consulted at this stage, a thorough history and the availability of diagnostics will help determine the outcome. The history can help determine the risk an animal is at for leptospirosis, such as contact with wild animals or potentially contaminated water sources. Routine bloodwork will not pick up a Leptospira infection, but can point towards a general bacterial infection that may be treated with appropriate antibiotics. The two of these together may lead a veterinarian to run a serology for leptospirosis, and treat accordingly. Once the disease has progressed to tissue damage the danger becomes more acute, not just for the animal but for the humans working or living with them, and medical intervention not just to treat the animal but establish quarantine protocols is imminently necessary.
While much of the pathology in the disease is concentrated on its occupation of the kidneys, the most common clinical presentation of advanced disease is due to liver damage. The pathogen migrates through the blood, which means large amounts of it can pass into and through the liver, causing wide spread damage. This pathology is evident in many of its common names, such as “rat-catcher’s yellows” and “black jaundice.” In ancient China it was the likely cause of “rice field jaundice.” The jaundice or icterus is caused by hepatocellular damage. This leads to the inability of the liver to process hemoglobin, causing a build-up of unconjugated bilirubin in the blood. However, the true danger is in compromise of the other functions of the liver, including toxin metabolism.
Currently there is no human vaccine for Leptospira recognized by the CDC, although there are other countries using them. Vaccines for dogs are in common use in the US, providing immunity for up to four known common serovars. Besides these measures, the best means of prevention is avoiding wild animal urine-through direct contact or through contaminated water, and controlling rodent populations which are considered lifetime reservoirs. As climate change affects areas of flooding and severe weather, further efforts will need to be made to control this already widespread disease.
References
Acevedo-Whitehouse K, Gulland FMD, Bowen L. MHC class II DRB diversity predicts antigen recognition and is associated with disease severity in California sea lions naturally infected with Leptospira interrogans. Infect Genet Evol. 2018;57:158-165
Leptospirosis; prevention; information; Adventure Racing – available at https://www.cdc.gov/leptospirosis/index.html Accessed Apr 5, 2019
Ben A. Leptospira and Leptospirosis – History of Leptospirosis and Leptospira. Current Topics in Microbiology and Immunology, 2015:387;1-9
Colombo VC, Gamietea I, Loffler SG et al. New host species for Leptospira borgpetersenii and Leptospira interrogans serovar Copenhageni. Vet Microbiol. 2018;215:90-92
Fávero JF, Fritzen A, Lovato LT et al. Immune response of a commercial vaccine against Leptospira interrogans: Antibodies and cytokine levels. Microb Pathog. 2018;114:46-49
Grosenbaugh DA, Pardo MC. Fifteen-month duration of immunity for the serovar Grippotyphosa fraction of a tetravalent canine leptospirosis vaccine. Vet Rec. 2018;182:665
Jorge S, Kremer FS, Oliveira NR et al. Whole-genome sequencing of Leptospira interrogans from southern Brazil: genetic features of a highly virulent strain. Mem Inst Oswaldo Cruz. 2018;113:80-86
Miotto BA, Tozzi BF, Penteado MS et al. Diagnosis of acute canine leptospirosis using multiple laboratory tests and characterization of the isolated strains. BMC Vet Res. 2018;14:222
Namroodi S, Shirazi AS, Khaleghi SR et al. Frequency of exposure of endangered Caspian seals to Canine distemper virus, Leptospira interrogans, and Toxoplasma gondii. PLoS One. 2018;13:e0196070
Wang Z, Jin L, Węgrzyn A. Leptospirosis vaccines. Microbial Cell Factories, 2007;6:39
Xu Y, Ye Q. Human leptospirosis vaccines in China. Human Vaccines & Immunotherapeutics, 2018;14:984-993

