Main Body
16. Receptor Regulation
Overview
- Intrinsic Regulation • receptors initiate regulation of a variety of events and are themselves subject to regulatory and homeostatic controls.
- Disease States • disease states can alter the number, function, and/or activity of receptors.
- Drugs • drugs can act as agonist, antagonists and allosteric modulators all of which can alter receptor function and number.
Intrinsic Regulation
Intrinsic Regulation • receptors are subject to regulation and homeostatic control. Left unregulated, receptors may be over stimulated, which may lead to pathological changes, including apoptosis. Therefore, regulation helps protect cells. There are times when an increased response is needed and others when a decreased response is preferred.
Cellular mechanisms of Increased Response
- Super/Hyper Sensitivity
- Synergism
- Upregulation
Super/Hypersensitivity • Super or hypersensitivity refers to an enhanced response to an agonist. Hypersensitivity may occur as a result of unmasking of receptors or accentuation of signal amplification.
- Unmasking of Receptors • some receptors have a masking protein covering the intracellular portion of a receptor, like the GPCR seen below for example. This masking protein prevents signal transduction and leads to decreased activity. When a masking protein in removed, activity increases.
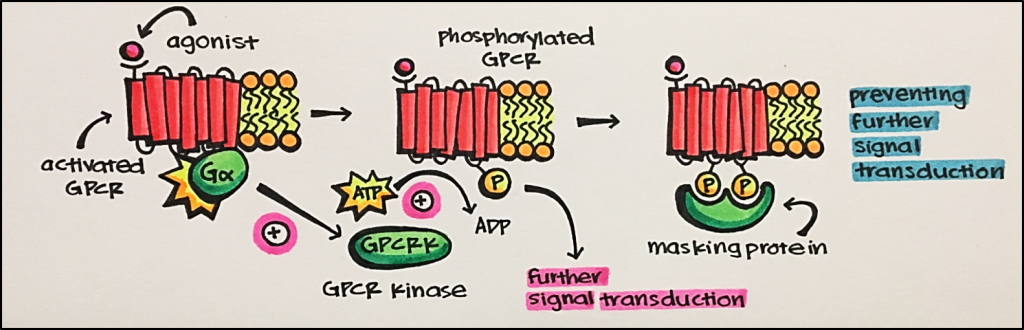
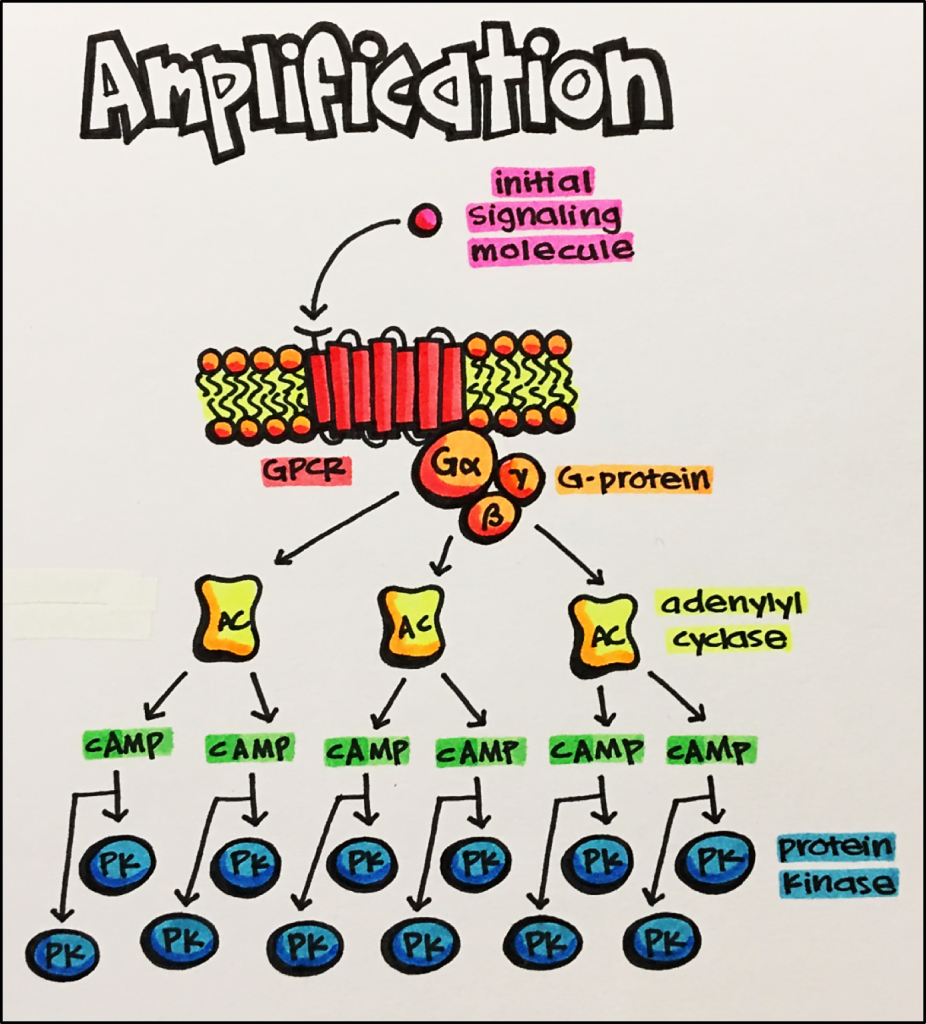
- Accentuation of Signal Amplification • this may occur with an increase in receptor phosphorylation or increased enzymatic activity. As was discussed earlier, phosphorylation can lead to the activation of a chain of second messengers and signal amplification. Therefore, as phosphorylation increases, so does signal transduction and amplification. Likewise, there are enzymes that catalyze components in a signal transduction pathway leading to increased signal transduction and amplification as well.The image below shows how signal amplification can be initiated by a single molecule. This particular example leads to the activation of protein kinases, which goes on to phosphorylate specific target molecules. As the signal is amplified, so is the amount of phosphorylation leading to an accentuation of signal amplification. If these kinases are not balanced by phosphatases, enzymes that reverse phosphorylation, phosphorylation can predominate and lead to further accentuation of the original signal.
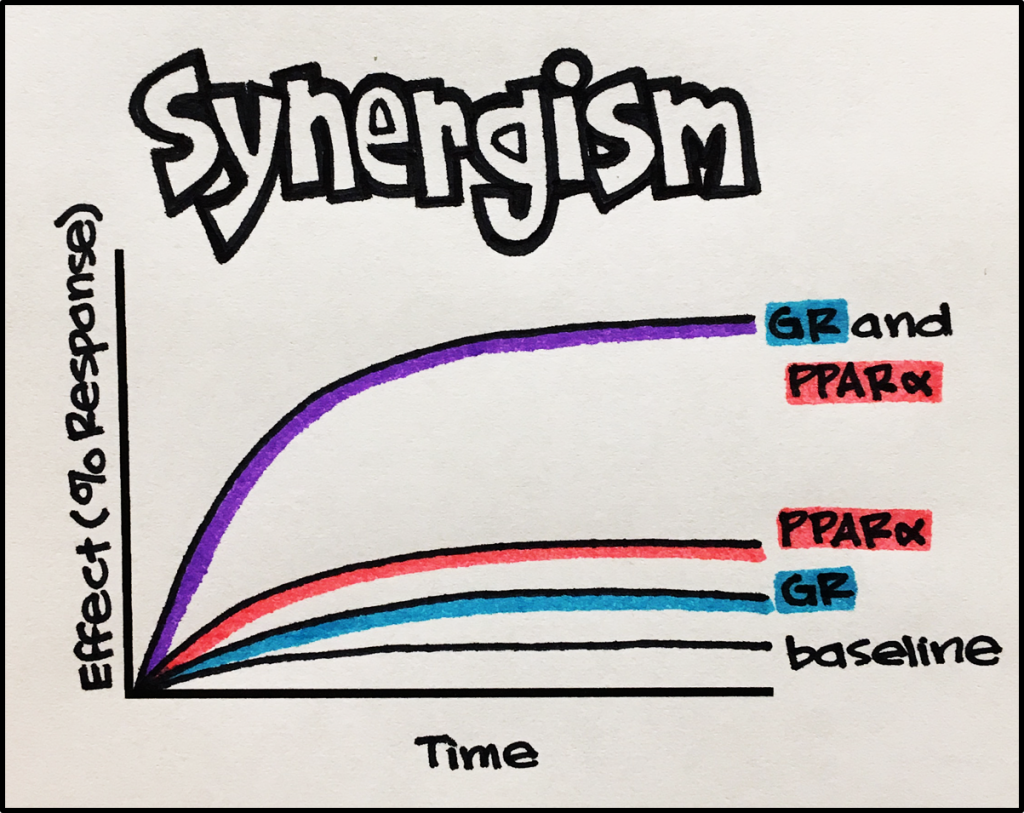
Synergism • when two receptors produce a combined effect that is greater than the sum of their individual effect.
Example • Glucocorticoids stimulate glucocorticoid receptors [GR], a type of nuclear receptor, resulting in increased erythroid cell (series of cell leading to red blood cells) production. When peroxisome proliferator-activated receptor alpha [PPARa] and GRs are stimulated simultaneously by their respective agonists, the resultant erythroid cell production is greater than the sum of production by each receptor individually. Together, PPARa and GR stimulation result in an enhanced response.
Upregulation • Upregulation refers to an increase in the number of receptors due to prolonged deprivation of receptors of interacting with their physiological neurotransmitter (e.g. by denervation of chronic use of a receptor antagonist). By expressing more receptors, there is a greater probability that a hormone will bump into and stimulate its receptor.
Cellular mechanisms of Decreased Response
- Desensitization
- Downregulation
- Tachyphylaxis
- Tolerance
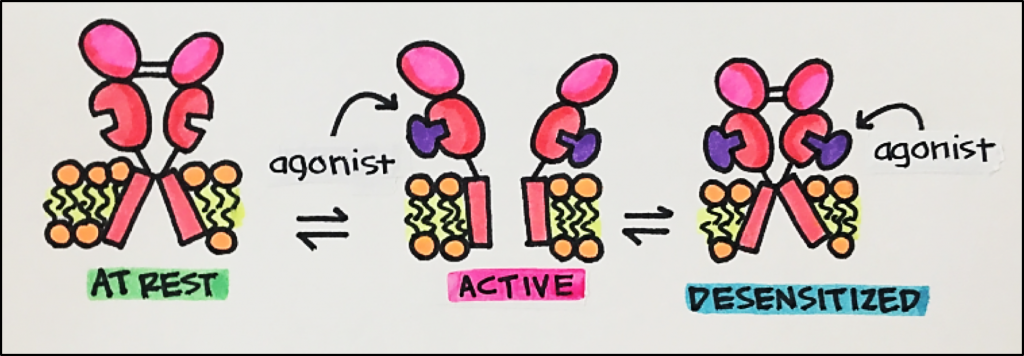
Desensitization • Desensitization refers to a reduced response to an agonist drug due to over activation of a receptor (high doses, prolonged exposure to agonist). There is a number of mechanisms of desensitization including: loss of receptor function through a decrease in receptor-coupled signaling components (e.g., G-proteins). Receptor desensitization may occur in the absence of significant changes in the number of receptors.
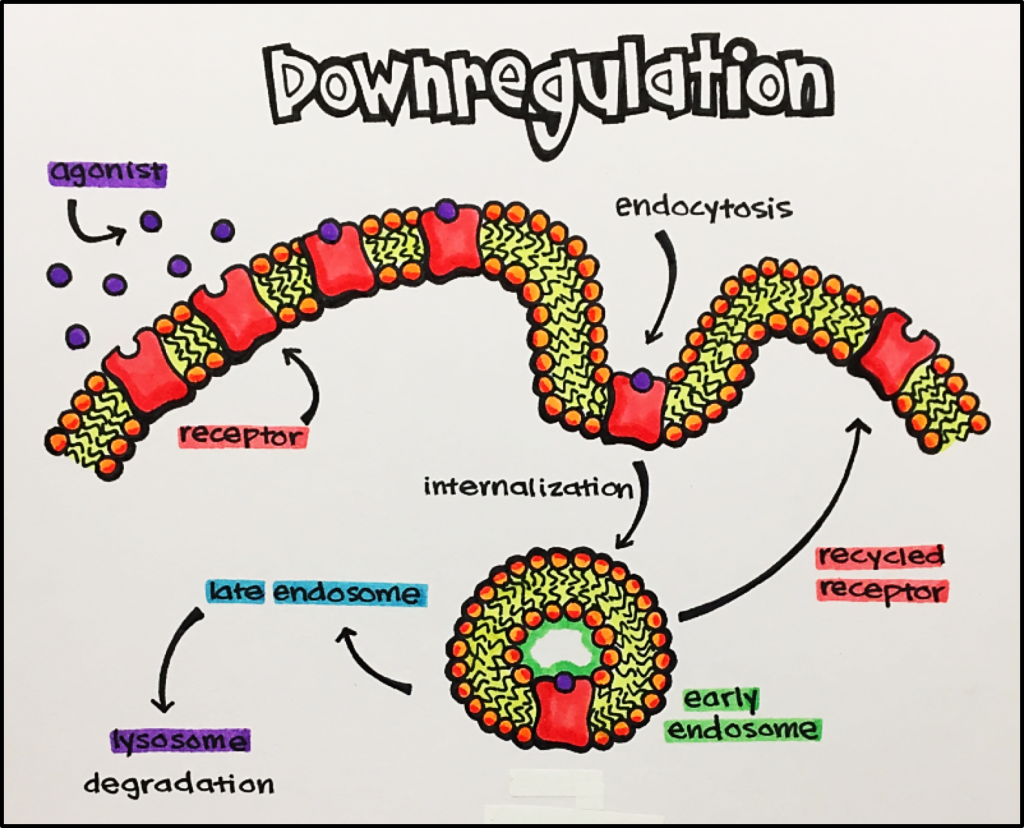
As the image shows, endocytosis involved the internalization of a receptor preventing it from carrying out signal transduction. A receptor may either go to the endosome then lysosome to be degraded or recycled back to the membrane surface to once again carry out signal transduction.
Tachyphylaxis • Tachyphylaxis is a rapid decrease in response to an agonist drug following repeated administration within a brief period; an acute form of desensitization. This can occur without a change in the number of receptors or the ability of a receptor to affect the downstream signaling molecules. Increasing the dose of the drug will not improve the response.
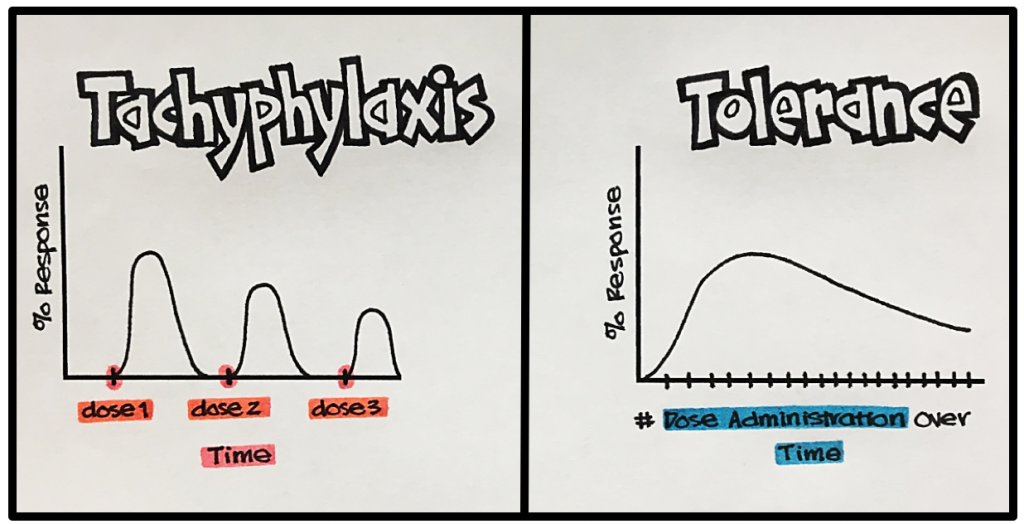
Tolerance • Tolerance refers to a gradual decreased response to a drug, requiring a higher dose of drug to achieve the same initial response. Tolerance is different from tachyphylaxis because it develops over a long period of time, whereas, tachyphylaxis is an acute event. In addition, tolerance can be overcome by increasing the dose, unlike tachyphylaxis.
Example • A great example of tolerance is in the story of Brett Favre, a Hall of Fame quarterback who played for the Green Bay Packers 1991-2010. In the midst of his career he developed an addiction to Vicodin (an analgesic medication that contains hydrocodone, an agonist of opiate receptors). He started taking two tablets to treat his sports-related injuries/pain and eventually worked his way up to 15 tablets due to a development of tolerance to Vicodin. At his worst, he was taking 14-days’ worth of Vicodin each day in order to achieve the same effect he originally had with 2 tablets, which contributed to his streak of 297 consecutive games played; currently the longest streak in NFL history by 27 games. You may read more about it at the link below:
Changes in receptor response by disease states
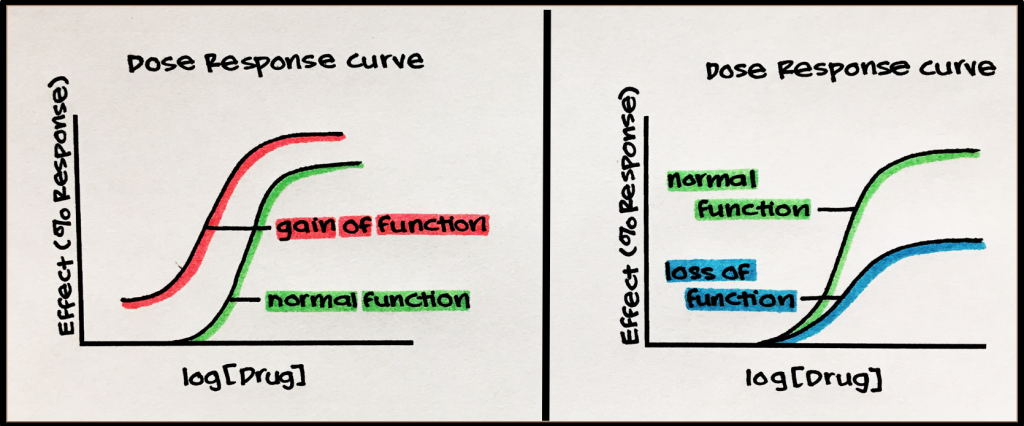
Disease states may alter the number of available receptors, which can alter the sensitivity and response of a given cell or tissue. Disease states may therefore alter the actual function or activity of those receptors; either through loss or gain of function.
Example • Loss of Receptors
Myasthenia Gravis is an autoimmune disorder in which antibodies destroy nicotinic acetylcholine receptors [nAChR] located in skeletal muscle. nAChRs help communicate signals resulting in muscle contraction. Thus, Myasthenia Gravis causes muscle weakness, droopy eyes and even difficulty in swallowing.
Myasthenia Gravis is treated with immunosuppressants to decrease the production of antibodies that destroy nAChRs as well as with acetylcholine esterase inhibitors [AChEIs] that prevent the breakdown of acetylcholine, a nAChR agonist, to increase its level in the synapse.
Example • Loss of Function • Androgen Receptors [AR]
Androgen receptors have variants caused by genetic mutations. These variants have varied levels of function, ranging from partial to complete loss of function. Individuals who have complete AR insensitivity exhibit Complete Androgen Insensitivity Syndrome [CAIS], and those who have partial AR insensitivity suffer from Partial Androgen Insensitivity Syndrome [PAIS]. Both syndromes cause a loss of receptor function.
Treatment for these syndromes includes hormone therapy; testosterone and/or dihydrotestosterone [DHT]. One great advantage of DHT over testosterone is that cannot be aromatized to estrogen, eliminating possible side effects associated with estrogen exposure.
Example • Gain-of-Function •A number of endocrine diseases are caused by gain-of-function mutations of GPCRs.
Type 2 Diabetes Mellitus [DM2] • DM2 can be associated with a gain-of-function mutation, resulting in increased expression of the a2A-adrenergic receptor; a GPCR that prevents or suppresses the secretion of insulin. As you can imagine, a patient with this gain-of-function mutation will have elevated blood glucose, potentially leading to type II diabetes mellitus.
Familial Hypocalcemia Hypocalciuria • This disease involves a gain-of-function mutation of the calcium-sensing receptor [CaSR]; a GPCR that allows the body to monitor and regulate the amount of calcium in the blood. This gain-of-function leads to increased sensitivity to calcium. Because CaSR maintains calcium homeostasis, its exaggerated response to calcium tells the body to excrete more calcium. This leads to decreased calcium levels in the blood (hypocalcemia) by suppressing the secretion of parathyroid hormone and increased renal excretion of calcium (hypercalciuria).

