1.9 Does the HPV vaccine lead to more sex in teenagers?
In the chapter introduction, we mentioned that many health professionals advocate vaccinating adolescents against HPV prior to the onset of sexual activity. The two most common forms of the vaccine (Cervarix and Gardasil) have been shown, through a series of long-term studies, to be effective at preventing most types of HPV[1]. However, some parents feel that selecting HPV vaccination for their kids is a way of giving their teenagers “permission” to be sexually active. Is there any evidence that this is the case? Specifically, does receiving the vaccine make an individual more likely to engage in sexual activity, especially at an early age?
In 2017, only 68.6% of adolescent females and 62.6% of adolescent males had initiated the vaccine sequence in the US. Even worse, only 53.1% of adolescent females and 44.3% of adolescent males had completed the three recommended doses[2]. These numbers fall far short of the 80% goal established by the U.S. Department of Health and Human Services. These rates are also far below the around 90% rates for other vaccines given in childhood like Tdap (tetanus, diphtheria, and pertussis) and MMR (measles, mumps, rubella).
These observations over parental hesitancy and vaccination rates led Rafael Meza and colleagues, in 2019, to question whether there was any difference in HPV vaccination and sexual behaviors in male and female college-aged students at the University of Michigan and college-aged participants living in Ann Arbor, Michigan[3].
HPV vaccination rates continue to increase. As of 2021, 76.9% of adolescents, ages 13-17 years, had begun the HPV vaccine and 61.7% had completed the recommended dosage [4].
Previous studies have found no link between HPV vaccination and sexual behavior. However, these studies mostly focused on adolescent and young adult females. This may be due to double-standards regarding what is expected and acceptable sexual behavior in females versus males. Meza’s group focused on sexual behaviors in females AND males. They hypothesized that choices regarding sexual behavior are not influenced by HPV vaccination status (whether an individual has received the HPV vaccine or not) and therefore predicted that vaccination status would have no association with sexual behavior.
Their experimental design included analysis of questionnaire data from 241 males and females ranging in age from 18-22 living in the Ann Arbor, Michigan area. Data was collected from 2015-2017.
To complete this analysis, researchers controlled for age, race, sex, and substance use. They then tested for a relationship between HPV vaccination status and occurrence of sexual debut (first experience of vaginal, oral, or anal sex), number of sexual partners, and age at sexual debut.
Check Yourself
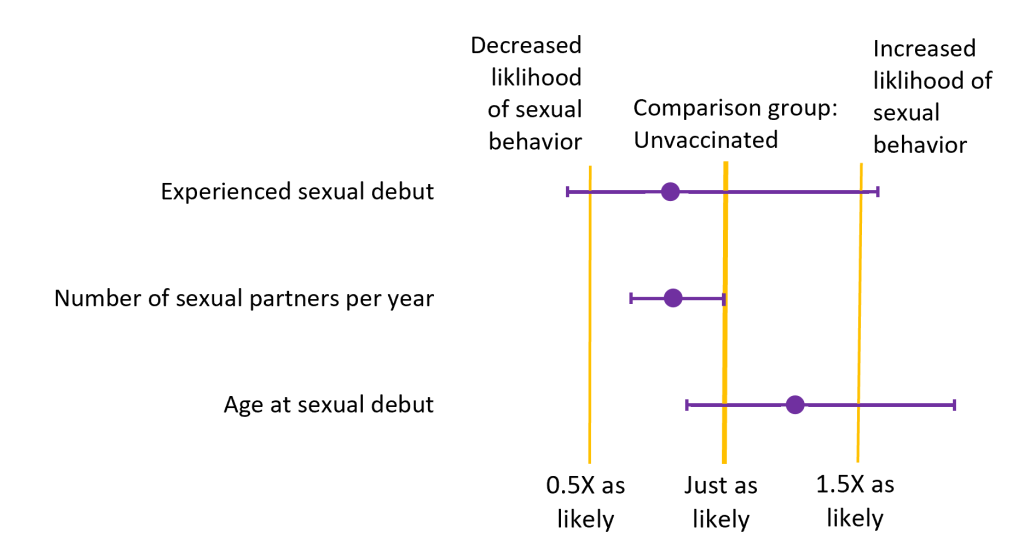
The figure contains the data, and now we need to identify trends or patterns and then interpret the data.
In Figure 1.10 we see that people in the study who had received the HPV vaccine were less likely to have experienced their sexual debut than folks who had not been vaccinated. However, you might also have noticed the 95% confidence interval overlaps with 1.0, meaning the two groups are actually similar in their likelihood of having had their sexual debut. They are so similar that we are not able to conclude that the likelihood of having experienced their sexual debut probability differs between people who are vaccinated and people who are not.
For the variable number of sexual partners per year, there is also a value less than 1.0. This means that vaccinated individuals had fewer sexual partners per year than the unvaccinated individuals. Again, the 95% confidence interval overlaps (just barely) with 1.0, meaning the two groups are actually similar in their number of sexual partners per year and we cannot conclude that the number of sexual partners varies between groups.
Lastly, we examine the age at sexual debut. We notice that folks that have received the HPV vaccine are more likely to be older at their sexual debut than those who have not received the HPV vaccine. Yet again, the 95% confidence interval overlaps with 1.0, meaning the two groups are similar in their age at sexual debut.
Therefore we would conclude that there is no difference in sexual behaviors between the two groups, vaccinated and unvaccinated. In other words, receiving the HPV vaccine does not make a person more likely to engage in sexual behaviors. This is consistent with our prediction and our hypothesis is supported. Receiving the HPV vaccine has no significant effect on sexual behavior.
Check Yourself
Meza’s studies have been supported by similar work refuting the idea that females who have received the HPV vaccine would be more likely to contract other sexually transmitted infections (such as chlamydia or herpes). In fact, a study by Tanya Mather and colleagues found that vaccinated women were more likely to have positive attitudes about safe-sex practices. Thus, the evidence collected so far seems to discredit the idea that HPV vaccination leads to more sex, or to risky sexual behavior.
Content on this page was originally published in The Evolution and Biology of Sex by Sehoya Cotner & Deena Wassenberg and has been expanded and updated by Katherine Furniss & Sarah Hammarlund in compliance with the original CC-BY-NC 4.0 license.
- Kash N, Lee M, Kollipara R, Downing C, Guidry J, Tyring S. Safety and efficacy data on vaccines and immunization to human papillomavirus. J Clin Med. 2015;4(4):614–33. ↵
- Walker TY, Elam-Evans LD, Yankey D, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2017. MMWR Morb Mortal Wkly Rep 2018;67:909–917. DOI: http://dx.doi.org/10.15585/mmwr.mm6733a1 ↵
- Brouwer AF, Delinger RL, Eisenberg MC, Campredon LP, Walline HM, Carey TE, Meza R. HPV vaccination has not increased sexual activity or accelerated sexual debut in a college-aged cohort of men and women. BMC public health. 2019;19(1):821-821. doi:10.1186/s12889-019-7134-1 ↵
- Pingali C, Yankey D, Elam-Evans LD, et al. National Vaccination Coverage Among Adolescents Aged 13–17 Years — National Immunization Survey-Teen, United States, 2021. MMWR Morb Mortal Wkly Rep 2022;71:1101–1108. DOI: http://dx.doi.org/10.15585/mmwr.mm7135a1 ↵

