Chapter 4 – Health Equity and the Built Environment
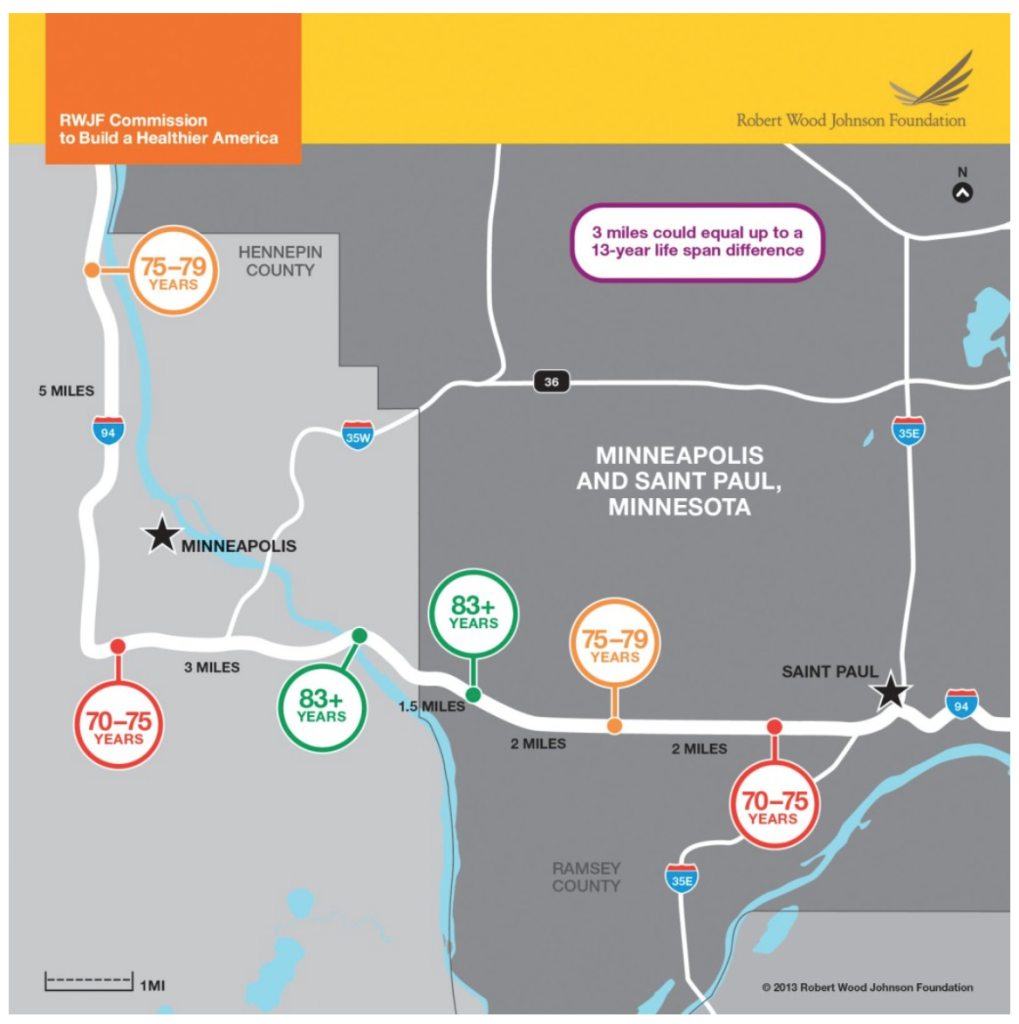
Metro Map: Minneapolis and St. Paul, MN Infographic by RWJF on RWJF.org
We will begin our exploration of the different equity fields with health equity. Health and health equity, as you will learn, encompass issues well beyond whether someone has fair access to medical care. We will learn that where you live has a major impact on how healthy you are and can be.
What is health? When we think of a healthy person we tend to focus on whether or not they are ill, what they eat, and their physical fitness. But human health refers to a much broader set of issues. Health can be described as:
…more than just the presence or absence of disease. It includes the overall well-being of an individual, the ability of an individual to fully participate in the social interactions of a community, and a lack of barriers to good health across a life span. (Lopez, 2012, p. 12)
Based on this description, what factors would you need to consider to call someone healthy? What does “overall well-being” mean to you? What allows someone to fully participate in the “social interactions of a community”?
As I write this I’m thinking about my 83-year-old mom as an example of a healthy person. If you met her you might be surprised (and I’m sure she would be very surprised that I chose her). She’s never been what you would call athletic and has some arthritis in her back, but she’s also almost impossibly positive about the world. She engages strangers in conversation wherever she goes. She wants to live as long as she can to see how the lives of each of her six children and 13 grandchildren and two great-grandchildren play out. She tries to eat well, goes to “gentle yoga” twice a week, and gets together with old friends. She goes to see her doctor regularly. She still drives to where she needs to go; she lives out in the suburbs so nothing is within easy walking distance. She’s lived in the same town for more than 45 years and knows lots of people close by. The ones she doesn’t know probably had my dad as a middle school teacher. So even beyond her friends and my sister and her family, who are just a few miles away, she has a really good network of people to support her. She doesn’t have to worry about the bills, she has a retirement savings, all of her kids are self-sufficient, and she doesn’t have to take care of any ailing family members.
People are often surprised to hear that someone’s zip code is a stronger predictor of health in the U.S. than their genetic code. Even if you didn’t know all of those things about my mom, you could have predicted that she is a healthy person by her zip code.[1] People are often surprised to hear that someone’s zip code is a stronger predictor of health in the U.S. than their genetic code. But as we have learned, where someone lives tells us a lot about their income level and social status. If my mom had continued living in the zip code in which she was raised, and at the same income levels as her parents, her health may not have been as good as it is today. But after my dad served in the Korean War my parents were able to use the GI Bill for my dad to attend college. My mom’s tuition was affordable (back when public universities were affordable), and they used an FHA loan to buy their first house together. Their incomes were thus higher than those of their parents, and as a result they had better access to healthcare and other things you need to stay healthy—including a safe home and neighborhood.
As we have learned from our readings on racial equity and post-WWII housing policy, people like my parents were lucky to be able to take advantage of federally subsidized low-interest loans and were not prevented from buying houses in suburban neighborhoods where homes steadily increased in value. Black families of the same generation, however, faced institutional and personal racism that prevented them from doing the same.
Our home was our financial safety net. If push came to shove, my parents could borrow against its steadily increasing value. I know there were times when they buckled down on household expenses, especially when my mom went to graduate school, but I don’t remember the lights going out or not having food in the fridge. I know my dad would have liked to change jobs after too many years as a middle school shop teacher, but he was better off than his friends who lost their jobs as factories closed down in the 1970s and 1980s and unemployment skyrocketed in our region. His job security was another federal benefit from the GI Bill.
Mental health is tied to physical health and both are tied to income.That feeling of relative security—or the absence of major stress related to finances—is another important connection between our health and where and how we live. Mental health is tied to physical health, and both are tied to income. If you are worried about paying the rent, feeding your family, or the safety of your neighborhood, your stress level increases. Stress is tied to obesity, high blood pressure, and other chronic illnesses. As stress goes up, immunities go down, and you are more likely to get sick. If your job has no sick days you may get fired if you miss work, and unemployment leads to more stress and poorer health. Stress also has prenatal impacts. High levels of the stress hormone cortisol during pregnancy can affect fetal neurological development.[2] While my siblings and I started with a big leg up because of our parents’ financial stability, some people start at a disadvantage even before they are born.[3]
This is the health-equity double whammy: if you have the resources to stay healthy—physically and psychologically—you are better able to advocate for yourself and make sure that you can stay healthy. If your landlord refuses to get rid of the asthma-triggering roaches, you can move. If you don’t connect well with your healthcare provider, you can get a second opinion or call a relative or friend who is in healthcare for some advice. But if you don’t have these resources, you will probably become less healthy over time. Your declining health will lead to declining opportunities to earn money. You may end up with even fewer resources, and in an even worse situation.
The Social Determinants of Health
As you will read in the Additional Resources section below, the social determinants of health include the conditions in which we live our lives, both physical and social: our economic stability, education, health and healthcare, neighborhood and built environment, and social and community contexts.[4] Only about 25% of our health is determined by genes, biology, and health behaviors. The other 75% relates to social determinants. Of those determinants, more than 40% of our health is determined by our physical environment. Some of the ways in which where we live impacts our health are highly visible: smog-covered cities, unsafe traffic crossings, a lack of parks for recreation and exercise, a lack of nearby health clinics or grocery stores, insect-infested apartments. Others are not as visible, like a lack of living-wage jobs, educational opportunities, social networks, and political power.
In other words, the place where you live is an indicator of your income level and social status, which are both key social determinants of health. And the place where you live—whether it has access to transit, parks, good schools, safe pedestrian environments, grocery stores, etc.—impacts your ability to be and stay healthy.
Environmental Design as a Prescription for Health
Over the past 20 years, environmental designers and health researchers have argued that a way of bridging the health gap, especially for chronic disease, is to focus on the built environment. They contend that if we had better sidewalks and more bike lanes and parks, people would exercise more. If grocery stores selling healthful foods were in every neighborhood, people would have better nutrition.
But recent evaluations of such measures are leading health researchers to believe that physical changes to neighborhoods, though important, are not enough. The same patterns of institutional and personal racism that tie people to low or middle-class housing and neighborhoods also impact their freedom to take advantage of possibilities that might improve their physical and mental health. Adding sidewalks, grocery stores, and parks to low-income neighborhoods, for example, may do little to change people’s health outcomes. These studies argue that we must also consider the interrelated issues of a person’s life choices (their agency) and life chances (the underlying social and economic structures within which each person lives). Going for a walk to get some exercise, buying and preparing healthful foods, relaxing in the park with family and friends after a stressful work week, are all life choices that help us stay healthy. But whether or not we can make the “right” choices depends on the structural issues of how much time, money, and status we have: our life chances.
Thus structure and agency interact, with agency playing a role in choosing courses of action among available options that are structured by resources, norms, and class circumstances (Blacksher Lovasi, 2012, p. 173).
“Structural” issues, like income, can severely limit someone’s ability to buy healthy foods, feel safe enough in their neighborhood to take a walk, and take time off work to see friends.
This is not to say that the built environment doesn’t matter to a person’s health. Rather, environment must be considered alongside agency and structure. Health can’t be environmentally determined; physical changes alone to a neighborhood won’t make the neighborhood’s residents healthier. That said, in the case of health issues related to pollution, physical changes can protect people’s health. People living in Flint, Michigan would not have lead poisoning if their water supply was safe. People would be less likely to be hit by cars if intersections prioritized pedestrian rather than vehicular movement. There are many opportunities to make broad changes and small improvements that would have a big impact on these kinds of environmental quality and safety-related issues.
Creating and maintaining safe and affordable housing and preventing displacement is a key component of any health equity approach.Other recent studies have pointed to a Catch-22 related to health equity and improvements in the built environment. Improving sidewalks, parks, and intersections, and adding bike lanes and grocery stores, can increase the value of adjacent properties. Home owners benefit from these improvements. But people who do not own their homes may face rent increases, especially as property taxes increase for their landlords. They may have to move, which destabilizes their social networks, brings on more stress, and may require a change in schools for kids and a longer commute to work. Consider what happens when a toxic waste site is cleaned up and turned into a park. This often leads to an increase in rents in the neighborhood, so that the people who had to live so long with these dangers of toxic waste don’t end up reaping the benefits of the safe, new amenities. Creating and maintaining safe and affordable housing and preventing displacement is a key component of any health equity approach.
Since health is such a robust equity measure, touching all aspects of people’s daily lives and the places where they live, it can seem almost impossible to imagine the kinds of changes that are needed to create health equity. How can we ensure that people have the agency to improve their health, and healthy environments in which to live? Some of the answers to these questions may lie in other equity fields, like housing, transportation and information equity. Other answers have yet to be identified or explored.
In “Reducing Health Disparities Through a Focus on Communities” (PolicyLink, 2002), the authors provide an overview of the social determinants of health and offer example strategies for addressing health disparities. As you read about these strategies, pay attention to the following questions: who might need to be involved in implementing them? What range of professional and community expertise is required? What barriers might arise? What is the relationship between changes to policies and changes to the built environments? What strategies might relate to the stories you heard in the “Unnatural Causes” video clips? Were there any issues raised in the videos that were not discussed in the report? In the next two chapters, we will read about transportation and information equity. Based on what you know about health equity, how would fair and just access to transportation and information help someone lead a healthier life?
As massive and intractable as the problems seem, there are many ways to contribute.By this point I imagine that your understanding of health has shifted. And because health is such an all-encompassing category, your view of the world may have shifted as well. You may also feel overwhelmed by the scale and complexity of the problem of health inequities. Take some time to reflect on who you are, and the skills and unique experiences you could use to contribute to ongoing work on health equity. As massive and intractable as the problems seem, there are many ways to contribute. You may already be volunteering at a community garden or food-shelf, or reading to elderly people in a nursing home. All of these small efforts matter. Now that you have read about bigger scale efforts like those set out in the PolicyLink report and in the “Healthy Lives for All” report, where do you see your skills and experiences as being of value?
Additional Resources:
- The “Reducing Health Disparities Through a Focus on Communities Report” from PolicyLink summarizes the social determinants of health and offers strategies for addressing health disparities in communities. Available at http://www.policylink.org/sites/default/files/REDUCINGHEALTHDISPARITIES_FINAL.PDF
- Dr. Renaisa Anthony, Deputy Director (CRHD) at the University of Nebraska Medical Center discusses the impact of race, gender, and background on health outcomes. Available at https://www.youtube.com/watch?v=ywQJGnzQKGs
- The clips from, “Unnatural Causes,” a film about health equity issues will add depth to our understanding of the different health issues facing different communities.
Available at https://www.youtube.com/playlist?list=PLEF0280B25D0841C4 - In the TEDxFargo talk by Dr. Donald Warne, you will learn about the health equity issues facing his community. How does Dr. Warne encourage us to define health? How does his definition of health relate to your own world view on health? What kinds of solutions might arise if health equity were addressed through this worldview?
Available at https://www.youtube.com/watch?v=3phTundagzQ
Works Cited
Blacksher, E. & Lovasi, G. S. (2012). Place-focused physical activity research, human agency, and social justice in public health: Taking agency seriously in studies of the built environment. Health & Place, 18(2), 172–179. https://doi.org/10.1016/j.healthplace.2011.08.019
Lopez, R. (2012). The built environment and public health. San Francisco, CA: John Wiley & Sons.
PolicyLink. (2002, November). Reducing health disparities through a focus on communities report. Available at http://www.policylink.org/sites/default/files/REDUCINGHEALTHDISPARITIES_FINAL.PDF
Endnotes
- See “Zip code better predictor of health than genetic code” at https://www.hsph.harvard.edu/news/features/zip-code-better-predictor-of-health-than-genetic-code/ ↵
- See “Acute stress in utero has negative effects later in life among poor children, Stanford sociologist finds” at https://news.stanford.edu/press-releases/2018/08/14/inequalities-prenatal-stress/ ↵
- See Braveman, P. & Gruskin, S. (2003). Defining equity in health. Journal of Epidemiology and Community Health, 57(4), 254. At https://jech.bmj.com/content/57/4/254.full.pdf ↵
- See Centers for Disease Control and Prevention Social Determinants of Health at https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html ↵

