Chapter 3 – Beta-lactams
Overview/Relevance
Groups of interest for swine antibiotherapy in the beta-lactam family are penicillins, extended-spectrum penicillins and cephalosporins of second and third generation.
Useful molecules to know in swine medicine:
- Penicillin
- Extended-Spectrum Penicillins: Amoxicillin
- Cephalosporin of 3rd generation: Ceftiofur
Mechanism of Action
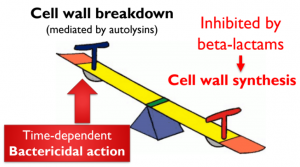
Peptido-glycans surrounds the bacterial membrane and give it its shape. Beta-lactams stop the polymerisation process. Because the bacterial membrane is in constant reshaping, there is an equilibrium between the polymerases creating the structure and the autolysins breaking it. Beta-lactams stop the polymerisation but not the lysis, therefore over time, liaisons between peptidoglycans are destroyed but not repaired and the cell membrane loses its structure. Eventually, the bacteria cell dies out.
Check your learning: Beta-lactams and mechanism of action
Spectrum
Penicillins have a narrow to moderate spectrum and are more effective towards Gram + bacteria than against Gram – bacteria. Cephalosporins have a moderate spectrum and are effective towards both Gram + and – bacteria. Mycoplasmas do not have a cell wall therefore they have an innate resistance against beta-lactams.

Check your learning: Beta-lactams and Spectrum
Absorption
Natural antibiotics easily broken down in the stomach, synthetics ones are more stable but overall poor oral bioavailability.
Distribution
Beta-lactams are weak acids, therefore they do not accumulate in the milk and are not first choice options to treat mastitis.
Penicillins and cephalosporins have a low volume distribution because they are water soluble.
This means that they have a low tissue penetration except in cases when there is inflammation ex: Brain Blood Barrier
Elimination
The half-life is short except for specific long-acting formulation such as ceftiofur crystalline free acid. Beta-lactams are mostly eliminated through the urine.
Adverse effects
Beta-lactams toxicity is low in swine. This tends to incite practitioners to increase the dose. This is counter-productive because beta-lactams are not concentration-dependent antibacterials and this practice could lead to more resistance in the future.
There are a lot of resistances against beta-lactams.
The most common are beta-lactamases which are enzymes that destroy the ring structure of antimicrobials and renders them useless. They can be part of the original genome of the bacteria or be acquired as a plasmid. Penicillins and extended-spectrum penicillins are the most susceptible to beta-lactamases. Cephalosporins, especially of the latest generations tend to be more resistant to them.
Other resistance mechanisms are changes in the peptido-glycans polymerase structure, a decrease in drug access, especially in Gram – bacteria. This can be achieved by decreasing the influx through the porines or increasing the efflux. Lastly, bacteria can circumvent the drug action by decreasing the autolysin activity.
