2.3 Pemphigus Foliaceus
-
General Considerations
- Pemphigus foliaceus is the most common autoimmune skin disease of dogs and cats.
- Akitas and Chow Chows may be predisposed.
Important Facts
- Pemphigus foliaceus is the most common autoimmune skin disease of dogs and cats.
-
Clinical Signs
- Lesions:
- Pustules are rarely seen because they are formed superficially in the skin (i.e. subcorneal) and, thus, rupture very easily. They are replaced by yellowish to light brown crusts.
- Lesions:

-
-
- Secondary lesions including crusts, scales, alopecia, erosions, and erythema are seen more often.
-

-
-
- Pruritus and pain are variable.
- Systemic signs are uncommon. Animals usually feel good; however, a few dogs become depressed, lethargic and anorexic.
- Distribution of lesions:
- Nose – Lesions frequently start on the face especially the dorsal aspect of the muzzle and may extend to the nasal planum, albeit rarely.
-


-
-
- Pinnae – The concave aspect of the pinnae is often affected. The convex aspect may be affected and, typically, in conjunction with the concave aspect.
-


-
-
- Footpads are often affected and lesions are characterized by hyperkeratosis (i.e. thickening of the stratum corneum), pustules, crusts, and erythema. Erosions form when adhered crusts are removed. Anecdotal reports suggest that footpads may be the only area affected in rare cases. However, the authors have not seem such cases.
-

-
-
- Generalized distribution may be seen in some cases.
- Paronychia, which is inflammation of the nail fold, is a common and unique feature of pemphigus foliaceus in cats. Purulent discharge and crusting are often present.
-

-
-
- Oral mucosal involvement is not seen in pemphigus foliaceus.
- Differential diagnoses include the pustular and crusting disorders listed below.
- Pemphigus erythematosus, superficial bacterial skin infection, pustular dermatophytosis, drug eruption, dermatomyositis, eosinophilic pustulosis, zinc responsive dermatitis, cutaneous epitheliotrophic T-cell lymphoma, superficial necrolytic dermatosis and distemper.
-
Important Facts
- Typical clinical signs include pustules (transient), yellowish-brown crusts (often seen), erosions, scales, and erythema localized to the dorsal of the muzzle, pinnae and footpads. However, not all these sites are affected in every case.
- Cats can develop inflammation of the nail folds (paronychia).
- Generalized involvement can occur.
- Oral mucosal involvement does not occur.
-
Diagnosis
- History – Usually acute onset and gradual progression.
- Clinical Signs:
- Yellowish-brown, honey-colored crusts are typically the most commonly seen lesions.
- Dorsal muzzle (may extend to the nasal planum), pinnae, and footpads are typically affected sites.
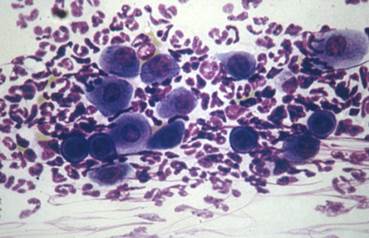
- Cytology of pustule content (if pustules are not present, collect sample from underneath crusts) reveals:
- Nondegenerate neutrophils, multiple rafts of acantholytic keratinocytes, +/- eosinophils. Bacteria may be seen if a secondary infection is present.
-
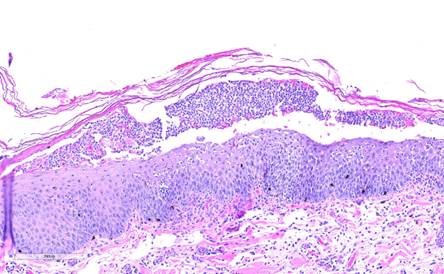
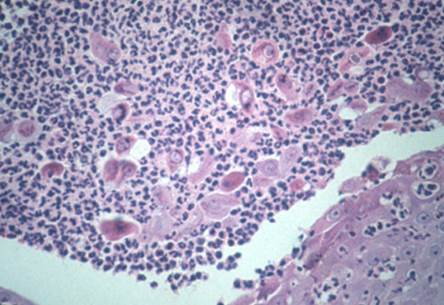
- Histopathology:
- Subcorneal or superficial intra-epidermal pustules with nondegenerate neutrophils, +/- eosinophils, and acantholytic keratinocytes. Bacteria are often absent. These histopathological findings with a characteristic history and clinical signs are diagnostic of pemphigus foliaceus.
- Histopathology:
-
-
-
- Read the histopathology description carefully for clues.
- Consider repeating the biopsy to obtain the diagnosis if your index of suspicion is high.
- Direct immunofluorescence and immunohistochemistry show intercellular staining of immunoglobulins. These tests are not available routinely.
-
-
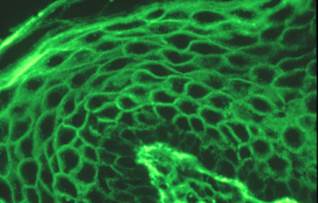
-
-
-
- Skin samples should be fixed in Michel’s solution for immunofluorescence or in formalin for immunohistochemistry.
- Remember! False negative results are common. False positives occur if nasal planum or footpads are submitted as samples.
- Indirect immunofluorescence shows the same staining pattern as for direct.
- Serum is submitted for this test.
- Remember! False negative results are common.
- CBC, chemistry profile, urinalysis:
- These tests are usually normal.
- Inflammatory changes such as leukocytosis may be seen.
- Antinuclear antibody test (ANA) should be negative but false positive results may occur. This test is not done if pemphigus foliaceus is the presumptive diagnosis.
-
-
Important Facts
- Compatible history and clinical signs (pustules and/or crusts on dorsal muzzle, pinnae, footpads) provide important diagnostic information.
- Cytological exam of direct smear from a freshly ruptured pustule or from the exudate present underneath crusts, reveal nondegenerate neutrophils, +/- eosinophils, and many acantholytic keratinocytes. If acantholytic keratinocytes are not present, the diagnosis of pemphigus foliaceus is less likely.
- Histopathology is the most important diagnostic test and reveals subcorneal pustules containing neutrophils, +/- eosinophils, and many acantholytic keratinocytes.
- Direct and indirect immunofluorescence or immunohistochemistry tests are not frequently used as a diagnostic tool because false negative results are common and these tests are not routinely available.
- Remember! Do not biopsy nasal planum or footpad lesions for direct immunofluorescence or immunohistochemistry tests because these sites are often positive in normal dogs (i.e. false positive).
- CBC can show leukocytosis.
- Antinuclear antibody test (ANA) is negative.
-
Treatment
- Options are a single or combination of the following drugs (See: “Therapy for Autoimmune Diseases” for dose, protocol, etc.).
- Glucocorticoids.
- Mycophenolate mofetil (dogs).
- Azathioprine (do not use it in cats because they will likely develop bone marrow suppression).
- Chlorambucil.
- Ciclosporin may be an option for cats. However, dogs do not seem to respond well to ciclosporin but it can be tried in selective cases at higher doses.
- Oclacitinib (Apoquel®) – Case reports have shown its efficacy to treat canine and feline pemphigus foliaceus.
- Gold salts are used when other treatments have failed.
- Options are a single or combination of the following drugs (See: “Therapy for Autoimmune Diseases” for dose, protocol, etc.).
References
Bizikova P, Burrows A. Feline pemphigus foliaceus: original case series and a comprehensive literature review. BMC Vet Res 2019; https://doi.org/10.1186/s12917-018-1739-y.
Carrasco I, Martinez M and Albinyana G. Beneficial effect of oclacitinib in a case of feline pemphigus foliaceus. Vet Dermatol 2021; 32:299-301.
Dalmau A, Ordeix L. Putative pemphigus-like reaction to oral fluralaner in a dog. Vet Dermatol 2023; DOI: 10.1111/vde.13243.
Diane E. Preziosi et al. Feline pemphigus foliaceus: a retrospective analysis of 57 cases. Vet Dermatol 2003; 14(6):313-321.
Lopes NL, Campos DR, Machado MA et al. A blinded, randomized, placebo-controlled trial of the safety of oclacitinib in cats. BMC Vet Res 2019; 15:137.
Medleau L, Hnilica KA. Chapter 8. Autoimmune and immune-mediated skin disorders. In: Small Animal Dermatology: A color Atlas and Therapeutic Guide 2006. 2nd ed. W.B. Saunders, Missouri, 189-227.
Miller, Griffin and Campbell. Chapter 9. Autoimmune and immune-mediated dermatoses. In: Muller & Kirk’s Small Animal Dermatology 2013. 7th ed., W.B. Saunders, Missouri; 432-462.
Olivry T. Auto-immune skin disease in animals: time to reclassify and review after 40 years. BMC Vet Res 2018; https://doi.org/10.1186/s12917-018-1477-1.
Olivry T, Chan LS. Autoimmune blistering dermatoses in domestic animals. Clin Dermatol 2001; 19(6):750-760.
Olivry T., Jackson HA. Diagnosing new autoimmune blistering skin diseases of dogs and cats. Clin Tech Small Anim Pract 2001; 16: 225-229.
Olivry T. Linder KE. Dermatoses affecting desmosomes in animals: a mechanistic review of acantholytic blistering skin diseases. Vet Dermatol 2009; 20: 313-326.
Outerbridge CA, Affolter VK, Lyons LA et al. An unresponsive progressive pustular and crusting dermatitis with acantholysis in nine cats. Vet Dermatol 2017; DOI: 10.1111/vde.12501.
Rosenkrantz WS. Pemphigus: current therapy. Vet Dermatol 2004; 15(2):90-98.

