1.5 Hypothyroidism – Canine
Learning Objectives
- Remember! Hypothyroidism is arguably the most common endocrine disorder of dogs. However, it is over diagnosed. Before clinical signs of hypothyroidism can develop, more than 75% of the thyroid gland parenchyma has to be destroyed.
- Keep in mind! More than 95% of hypothyroidism cases you will deal with in practice will be caused by primary hypothyroidism (likely lymphocytic thyroiditis or idiopathic atrophy of the thyroid parenchyma).
- Remember! Hypothyroidism occurs more often in middle age to old dogs (4 to 8 year old dogs). Because thyroid hormones are important in cell metabolism, almost every organ system in the body can be affected resulting in quite variable clinical signs. This makes clinical diagnosis a challenge.
- Know the common and uncommon clinical signs associated with canine hypothyroidism.
- Remember! The diagnosis of hypothyroidism should be based on a characteristic history, physical findings, clinicopathologic abnormalities, and thyroid functional tests. Do not rely solely on the thyroid tests to make a diagnosis of hypothyroidism as many non-thyroidal factors can affect the tests results.
- Remember! The clinicopathologic abnormalities are not specific for hypothyroidism and should only be used to support a presumptive diagnosis. Know the clinicopathologic abnormalities associated with hypothyroidism.
- Keep in mind! Total T4 measurement includes measuring the protein bound fraction and the free fraction of the hormone. It is the most commonly requested diagnostic test because it is inexpensive, involves only one blood sample collection, and the assay is widely available. However, non-thyroidal illnesses and various drugs can lower total T4 levels and suggest hypothyroidism to veterinarians who may not be aware of this fact.
- Know the non-thyroid diseases and the commonly used drugs that can lower total T4 concentrations.
- Know the accuracy of fT4 measurement by equilibrium dialysis to diagnose hypothyroidism.
- Know the accuracy of endogenous TSH measurement to diagnose hypothyroidism. Know what the TSH values should be in most dogs with hypothyroidism (i.e. normal, high or low).
- Remember! Total T4, fT4 by equilibrium dialysis and endogenous TSH can be affected by non-thyroidal illness and drugs; however, total T4 is more affected than fT4 by equilibrium dialysis and both are more affected than endogenous TSH.
- Know the value of measuring serum total T3 concentration to diagnose hypothyroidism and justify your answer. Know the main value of requesting serum total T3 concentration.
- Learn the situation where requesting a TRH stimulation test can be of value.
- Know the accuracy of the TSH stimulation test to diagnose hypothyroidism. Would you have this test performed now? Why?
- Remember! A treatment trial can be done if the dog has signs of hypothyroidism but the test results are inconclusive. Recheck your patient during the trial and critically observe response to therapy. Lethargy and exercise intolerance should resolve in 7 to 10 days in most dogs, so call the client at this time period. Most other signs should significantly improve or resolve after 12 weeks of therapy.
- Keep in mind! Hypothyroidism is a challenging disease to diagnose. The diagnosis should be based on a complete history, clinical signs, and thyroid function test results. Currently, laboratories are routinely measuring not only total T4 but also fT4 by equilibrium dialysis and endogenous TSH. Therefore, you have the option of having these three hormones measured on a single blood sample.
- Know how to treat hypothyroidism including how to monitor response to therapy.
-
General Considerations
- Hypothyroidism is arguably the most common endocrine disorder of dogs.
- Before an animal can develop clinical signs of hypothyroidism, more than 75% of the thyroid gland parenchyma has to be destroyed.
- Canine hypothyroidism is a diagnostic challenge because of the wide variation in clinical signs.
- Extra-thyroidal influences such as systemic diseases (i.e. non-thyroidal illnesses or euthyroid sick syndrome) and drug therapies (e.g. glucocorticoids, potentiated sulfas etc.) have significant effects on thyroid hormone levels.
- Many different assays and function tests have been developed in an attempt to identify the most sensitive and specific thyroid test for hypothyroidism.
- Hypothyroidism is overdiagnosed in dogs. Unfortunately, many dogs are treated with thyroid supplements unnecessarily.
- Sight hounds have been reported to have reduced serum total T4 concentration compared to other breeds.
Important Facts
- Hypothyroidism is arguably the most common endocrine disorder of dogs.
- Before an animal can develop clinical signs of hypothyroidism, more than 75% of the thyroid gland parenchyma has to be destroyed.
- The extra-thyroidal influences such as systemic diseases and certain drugs have significant effects on thyroid hormone concentrations.
- Hypothyroidism is overdiagnosed. As a result many dogs are treated with thyroid supplements unnecessarily.
-
Etiology
- Hypothyroidism may develop due to a defect at any level of the hypothalamic-pituitary-thyroid gland axis and it can be acquired or congenital.
- More than 95% of the cases are caused by primary hypothyroidism (i.e. thyroid gland defect).
- Lymphocytic thyroiditis and idiopathic atrophy of the thyroid gland parenchyma are the most common causes of primary hypothyroidism in dogs.
- Lymphocytic thyroiditis is an immune-mediated disorder and the presence of circulating serum thyroglobulin autoantibodies (TGAA) is a marker for the disease. However, the mere presence of TGAA does not equate to hypothyroidism. One study, followed-up 171 TGAA positive dogs for 1 year. About 20% developed one or more thyroid hormone abnormalities and 5% developed frank hypothyroidism. It is recommended to follow up the TGAA positive dogs closely but do not treat a positive dog that does not have clinical signs of hypothyroidism.
- In idiopathic atrophy of the thyroid gland progressive reduction in the size of the thyroid follicles and replacement of the degenerating follicles with adipose tissue occur. Degeneration of the thyroid follicle cells is seen histologically early in the disease process.
- Neoplastic destruction is a rare cause of primary hypothyroidism. Clinical signs of hypothyroidism may develop following destruction of more than 75% of the normal thyroid gland by an infiltrative tumor. Thyroid carcinomas and squamous cell carcinoma are the most common tumors causing extensive destruction of the thyroid gland. Thyroid carcinomas or adenomas are usually hormonally inactive and, as a result, clinical signs of hyperthyroidism are uncommon.
- Congenital hypothyroidism is much less common than the acquired form and can result from thyroid hypoplasia or aplasia, and dysgenesis or dyshormonogenesis. Many of the reports are not well documented.
- The best example of congenital dyshormonogenesis is the nonsense mutation in the thyroperoxidase (TPO) gene in toy fox terriers and rat terriers resulting in congenital hypothyroidism associated with goiter (hyperplastic thyroid follicles). The trait is autosomal recessive and a genetic test to identify carriers is available.
- Another form of congenital dyshormonogenesis with goiter was reported in two members of a family of Shih-Tzu dogs. A sodium/iodide symporter gene mutation (SLC5A5) was identified in the affected siblings.
- Another well-characterized form of congenital hypothyroidism occurs in German shepherd dogs (and related breeds) with pituitary dwarfism.
- Less than 5% of the cases are caused by secondary (pituitary) or tertiary (hypothalamic) hypothyroidism.
Important Facts
- More than 95% of the cases are caused by primary hypothyroidism, which entails the involvement of the thyroid gland (i.e. at least 75% destruction by disease or abnormal hormone synthesis).
- Lymphocytic thyroiditis and idiopathic atrophy of the thyroid follicles are the most common causes of adult-onset primary hypothyroidism.
- The presence of serum TGAA is a marker for lymphocytic thyroiditis; however, only treat a positive case if clinical signs of hypothyroidism have developed.
- Toy Fox Terries and Rat Terries have an inherited form of congenital hypothyroidism and a genetic test to identify carriers is available.
-
Clinical Signs
- Signalment:
- Age – Hypothyroidism occurs most commonly in middle age to older dogs (range: 4 to 8 years old dogs; mean: 7 years).
- Hypothyroidism can occur in any breed; however, breeds reported to be predisposed include Giant Schnauzer, Borzoi, Cocker Spaniel, Great Dane, Irish Wolfhound, Boxer, Rhodesian Ridgeback, Irish Setter, Golden Retriever, Doberman Pinscher, and English setter. Be aware that Sighthounds typically have T4 levels lower than most laboratory reference ranges.
- Sex – No sex predilection reported.
- Classical signs – Most dogs will present with dermatologic and metabolic signs.
- Dermatologic signs:
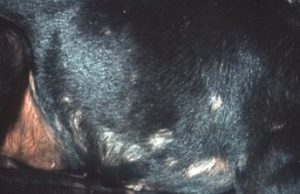
- Symmetrical, non-pruritic, non-inflammatory alopecia and hyperpigmentation of the trunk.
- Dermatologic signs:
- Signalment:



-
-
-
- Alopecia of the distal half of the tail – “rat tail”.
-
-

-
-
-
- Alopecia associated with hypothyroidism typically spares the face and distal extremities; however, some dogs develop non-inflammatory alopecia and hyperpigmentation on the dorsal aspect of the muzzle.
-
-


-
-
-
- Secondary seborrhea, comedones, and superficial pyoderma are common in hypothyroidism. Dogs with secondary superficial pyoderma may become itch.
-
-

-
-
-
- Another dermatologic finding occurs when excessive amounts of proteoglycans (i.e. mucopolyssacharides associated with protein) accumulate in the dermis, causing the myxedematous appearance (i.e. tragic facial expression) present in some patients with chronic disease.
-
-

-
-
- Metabolic signs:
- Obesity – It is a manifestation of low metabolic rate. The degree of obesity is usually moderate, although obesity without polyphagia is the presenting complaint in some hypothyroid animals.
- Cold intolerance – It is a manifestation of low metabolic rate.
- Lethargy – It is a manifestation of low metabolic rate. The presence of lethargy is frequently overlooked in hypothyroid dogs. Owners only notice the pet’s lethargy after thyroid hormone supplementation results in increased activity and alertness.
- Weakness and exercise intolerance – These signs can result from the general metabolic derangements that occur in hypothyroidism or may be an indication of a neuropathy or myopathy.
- Lethargy, weakness, and exercise intolerance generally resolve within 2 weeks of initiating treatment unless a neuropathy is present.
- Cardiovascular abnormality – Bradycardia, a weak apex beat, and poor pulse quality. Low-voltage electrocardiographic complexes occur in more than 50% of hypothyroid dogs and myocardial contractility is often mildly impaired.
- Many cases do not exhibit classical signs.
- Metabolic signs:
-
Important Facts
- Most dogs will present with dermatologic and metabolic signs.
- Typical signs include symmetrical, non-pruritic, non-inflammatory alopecia and hyperpigmentation of the trunk, obesity without increased appetite, lethargy, weakness, and cold intolerance, but these signs may not be always present.
- Secondary seborrhea and superficial staphylococcal pyoderma are common, which can result in skin inflammation and pruritus.
-
- Uncommon Signs:
- Neuropathy:
- Localized neuropathies may occur, resulting in facial and vestibular signs, megaesophagus, and laryngeal paralysis. Hypothyroidism does not appear to be involved in the pathogenesis of most cases of laryngeal paralysis. The abnormal thyroid hormone levels present in some cases of laryngeal paralysis is most likely due to euthyroid sick syndrome.
- Generalized neuropathy can result in progressive generalized weakness, depression, proprioceptive deficits, and hyporeflexia.
- Euthyroid dogs with neuropathy or megaesophagus may have suppressed serum T4 and T3 levels, so establishing a diagnosis of hypothyroidism in these cases is problematic.
- Central nervous system signs:
- Ataxia, hemiparesis, hypermetria, head tilt, nystagmus, circling, and dysfunction of multiple cranial nerves can occur with hypothyroidism.
- The cause is unknown. Thyroid hormone supplementation results in improvement or complete resolution of signs.
- Cerebrovascular atherosclerosis and associated hypoxia or infarction can result in central nervous system disease in hypothyroid dogs.
- Myxedema stupor or coma:
- It is a rare and life-threatening consequence of severe/chronic hypothyroidism in adult dogs.
- Signs consist of hypothermia without shivering, marked depression, bradycardia, hypotension, hypoventilation, non-pitting edema (i.e. myxedema due to excessive accumulation of proteoglycans in the dermis), and coma in addition to the common signs of hypothyroidism.
- Reproductive abnormalities:
- Reproductive abnormalities associated with hypothyroidism have been poorly documented.
- Overall, hypothyroidism is over diagnosed as a cause of reproductive abnormalities.
- Ocular abnormalities:
- Corneal lipid dystrophy, corneal ulcers, anterior uveitis, and retinopathies have been found in hypothyroid dogs. At this time, it is not known if these ocular abnormalities are caused by hypothyroidism.
- Corneal lipid dystrophy reported with hypothyroidism is probably an effect of hyperlipidemia rather than a direct result of thyroid hormone deficiency.
- Hypothyroidism should be considered as only one of several causes of hyperlipidemia associated with corneal lipid deposition.
- Neuropathy:
- Uncommon Signs:
Important Facts
- Uncommon signs of hypothyroidism include localized or generalized neuropathies, megaesophagus, central nervous system disease, myxedema stupor or coma, reproductive abnormalities, and ocular abnormalities.
- Euthyroid dogs with neuropathy or megaesophagus have been shown to have suppressed serum T4 and T3 levels, so establishing a diagnosis of hypothyroidism in these cases is problematic.
-
Diagnosis
- History and clinical signs.
- Clinicopathologic abnormalities:
- Nonspecific.
- Complete blood cell count (CBC) – Mild normocytic, normochromic, non-regenerative anemia is present in about 30%-40% of the cases.
- Chemistry profile:
- Thyroid hormones are important for all aspects of lipid metabolism including synthesis, mobilization and degradation with the most impact in reducing degradation.
- Fasting hypercholesterolemia is present in more than 75% of the cases.
- Fasting hyperlipidemia and hypertriglyceridemia are also common.
- Fasting hypercholesterolemia and hypertriglyceridemia can be associated with several other disorders. However, their presence in a dog with appropriate clinical signs is supportive evidence for hypothyroidism.
- Larger increases in cholesterol are more suggestive of hypothyroidism than non-thyroidal illness.
- Thyroid hormones are important for all aspects of lipid metabolism including synthesis, mobilization and degradation with the most impact in reducing degradation.
- Thyroid functional tests:
- Serum total T4 measurement:
- Serum total T4 measurement represents the sum of the protein-bound (more than 99% of the secreted T4) and free levels circulating in the blood.
- It is a useful screening test for hypothyroidism. Because most dogs with hypothyroidism (90%-100%) will have low total T4, a normal value can rule out hypothyroidism in most cases.
- Remember! Serum total T4 level is below normal reference intervals not only in hypothyroid dogs but also in dogs with normal thyroid function (i.e. euthyroid dogs). Therefore, its specificity is low (about 75%).
- The most common situations in which serum total T4 concentration is decreased in euthyroid dogs are:
- Systemic non-thyroidal illness:
- In general, the severity of illness and nutritional status appear to be the chief factors associated with decreased serum T4 concentrations.
- The decrease in serum T4 level is the body’s attempt to conserve metabolic resources in the face of disease.
- Diseases which have been associated with low basal T4 levels are: renal failure, liver disease, diabetes mellitus, Cushing’s syndrome, severe deep pyoderma, and generalized demodicosis.
- Total T4 is the second thyroid hormone most frequently lowered by non-thyroidal illness after total T3.
- Certain drugs:
- Glucocorticoids, potentiated sulfas (inhibit the synthesis of T4 and T3), phenobarbital, primidone, furosemide, salicylates, phenylbutazone, phenothiazines, radiographic contrast agents, flunixin meglumine, mitotane, diazepam, heparin, imidazoles, clomipramine, propanolol, penicillins and others. Glucocorticoids, potentiated sulfas and some non-steroidal anti-inflammatory drugs have been investigated in dogs but the other ones are extrapolated from human studies.
- Other factors:
- Age – The serum concentration of total T4 decreases with advanced age and may be below the normal reference interval in old dogs.
- Breed – Euthyroid sighthounds can have T4 concentrations at the hypothyroid reference interval.
- In conclusion:
- Low basal T4 values require further evaluation of the thyroid function. This is particularly true in dogs with unusual signs of hypothyroidism such as neuropathy or megaesophagus and dogs with severe illness or taking drugs known to lower total T4 concentrations.
- However, in the absence of concurrent therapy or other relatively severe illness, measurement of a very low T4 concentration in a dog with signs of hypothyroidism should suffice to diagnose the disease.
- Measuring serum cholesterol levels and complete blood cell count may add value to the measurement of basal T4 levels.
- Systemic non-thyroidal illness:
- Serum total T4 measurement:
Important Facts
- Normal basal T4 rules out hypothyroidism in most dogs.
- Low basal T4 is associated with not only hypothyroidism but also with systemic illness and various medications.
- Healthy sighthounds typically have serum T4 concentration below the normal reference intervals.
- Low serum T4 values require further evaluation of the thyroid function.
- In the absence of concurrent drugs or relatively severe non-thyroidal illness, the measurement of low T4 concentration in a dog with signs of hypothyroidism should suffice to make a definitive diagnosis.
-
-
- Serum total T3 measurement: It is not a very reliable test!
- Hypothyroid dogs often have normal or elevated T3 concentration.
- At least 40% of hypothyroid dogs with positive TGAA also had T3 autoantibodies, which spuriously increases serum T3 concentration when solid phase assays are used.
- Most of the serum T3 is derived from peripheral deiodination of T4; therefore, circulating serum T3 concentration does not reflect cellular concentrations.
- Serum T3 is the hormone most often affected (lowered) by non- thyroidal illness so, a low total T3 concentration may be more indicative of non-thyroidal illness than hypothyroidism.
- Serum T3 level is a poor indicator of thyroid function.
- Serum total T3 measurement: It is not a very reliable test!
-
Important Facts
- Hypothyroid dogs often have normal or elevated T3 concentration.
- T3 autoantibodies may spuriously increase the serum T3 concentration.
- Low T3 is more indicative of non-thyroidal illness than hypothyroidism.
- Serum T3 level is a poor indicator of thyroid function.
-
-
- Serum free T4 measurement:
- Greater than 99% of T4 is bound to plasma proteins.
- The unbound or free T4 (fT4) is biologically active because of its ability to diffuse into tissues, penetrate cell membranes, and interact with receptors.
- In theory, an accurate measurement of fT4 would transcend the effects that non-thyroidal illness and drugs have on total T4 concentration and give a more accurate indication of the thyroid gland status.
- Measurement of fT4 by radioimmunoassay (RIA) has shown little or no advantage over measurement of total T4 in diagnosing hypothyroidism.
- Measurement of fT4 by equilibrium dialysis is considered the gold standard test to measure fT4. One advantage of measuring fT4 by equilibrium dialysis over total T4 is that it is not affected by the presence of T4 autoantibodies.
- One study showed that fT4 measured by equilibrium dialysis remained normal in most cases with a reduction in total T4 and total T3 concentrations induced by non-thyroidal illness. Therefore, free T4 concentration measured by equilibrium dialysis are unlikely to be affected by non-thyroidal illness unless it is severe.
- Remember that concentrations of serum fT4 can also be lowered by drugs such as glucocorticoids, potentiated sulfas, and anticonvulsants.
- Before conclusions can be drawn more studies need to be conducted to verify the effects of non-thyroidal illness and drugs on serum fT4 concentrations measured by equilibrium dialysis.
- Serum free T4 measurement:
-
Important Facts
- Measurement of fT4 by equilibrium dialysis is considered the gold standard test to measure fT4 and it is not affected by the presence of T4 autoantibodies.
- Measurement of fT4 by equilibrium dialysis is typically not affected by non-thyroidal illness unless it is severe.
- Remember that concentrations of serum fT4 can also be lowered by drugs such as glucocorticoids, potentiated sulfas, and anticonvulsants.
- Before conclusions can be drawn more studies need to be conducted to verify the effects of non-thyroidal illness and drugs on serum fT4 levels measured by equilibrium dialysis.
-
-
- TSH stimulation test – It measures the thyroid gland hormone reserve.
- The TSH stimulation test is an accurate test to diagnose hypothyroidism; however, its high cost limits its use as a diagnostic test.
- Test interpretation:
- If a dog is normal, the 6-hour post-TSH T4 concentration should at least double the pre-value and fall within the laboratory normal range or the post-TSH T4 concentration should be higher than 45 nmol/L.
- If a dog is hypothyroid, little or no increase in the 6-hour post-TSH T4 concentration should be expected or the post-TSH T4 concentration should be lower than 15 nmol/L.
- Test protocol:
- Blood sample for measurement of serum total T4 should be obtained before and 6 hours after intravenous (IV) administration of recombinant human TSH (rhTSH) (Thyrogen®) at the dose of 75 or 150 µg. A study showed that the 150 µg dose should be used to better differentiate hypothyroidism from non-thyroidal illness or the effect of drugs on thyroid function.
- Each vial of rhTSH contains 0.9 mg of TSH and costs about $1,350.00. Doses can be aliquoted and frozen at -20°C for 12 weeks or stored at 4°C for 4 weeks.
- Disadvantages of the TSH stimulation test:
- High cost of rhTSH.
- Bovine TSH is no longer commercially available as a pharmaceutical preparation.
- It is a 6-hour test.
- TSH stimulation test – It measures the thyroid gland hormone reserve.
-
Important Facts
- The TSH stimulation test is an accurate test to diagnose hypothyroidism.
- However, the test is very expensive (rhTSH is expensive) and it is a 6-hour test.
-
-
- Endogenous TSH assay:
- Test interpretation:
- Primary hypothyroidism – It accounts for >95% of canine cases.
- Endogenous TSH concentrations should be above the reference intervals because the low circulating and pituitary T4 concentrations should result in increased TSH secretion (inhibition of pituitary negative feedback mechanism).
- Secondary (i.e. pituitary level) or tertiary hypothyroidism (i.e. hypothalamic level) – It accounts for <5% of canine cases.
- Endogenous TSH should be at the assay limit of detection (pituitary is not producing or is producing low amounts of endogenous TSH).
- Primary hypothyroidism – It accounts for >95% of canine cases.
- Accuracy of the test:
- In people, most non-thyroidal illnesses cases are associated with normal or decreased serum TSH concentrations.
- Recent studies in dogs showed that 20% to 40% of hypothyroid cases have normal serum endogenous TSH concentrations instead of the expected high levels.
- 15% of dogs with non-thyroidal illness have elevated serum TSH concentrations, which overlap with values measured in hypothyroid dogs.
- Dogs treated with potentiated sulfas had increased TSH after about 3 weeks of treatment and serum values returned to the normal range within about 3 weeks after stopping therapy.
- In summary:
- The current findings suggest that serum TSH concentration is not very sensitive to diagnose hypothyroidism because about one-fourth of hypothyroid dogs have values within the normal reference interval. However, it is more specific than total T4 and fT4 by equilibrium dialysis because it is less affected by non-thyroidal illness and drugs.
- Because endogenous TSH measurement has low sensitivity, it should not be used as the sole test to diagnose hypothyroidism. However, because it is less affected by non-thyroidal illness and drugs, it can be combined with total T4 and fT4 by equilibrium dialysis to increase their specificities.
- Advantages of the endogenous TSH assay:
- Only one blood sample is required.
- The test is cheaper than the TSH stimulation test.
- Test interpretation:
- Endogenous TSH assay:
-
Important Facts
- Endogenous TSH should be higher than normal in dogs with primary hypothyroidism.
- Unfortunately, recent studies showed that 20% to 40% of dogs with hypothyroidism have normal serum endogenous TSH concentrations indicating that this test is not sensitive to diagnose hypothyroidism.
- Endogenous TSH measurement is more specific than total T4 and fT4 by equilibrium dialysis because it is less affected by non-thyroidal illness and drugs.
- Because endogenous TSH measurement has low sensitivity, it should not be used as the sole test to diagnose hypothyroidism. However, because it is less affected by non-thyroid illness and drugs, it can be combined with total T4 and fT4 by equilibrium dialysis to increase their specificities.
-
-
- TRH stimulation test – It is not accurate to diagnose primary hypothyroidism.
- The measurement of total T4 after the exogenous administration of TRH is not an accurate test to diagnose hypothyroidism.
- Normal dogs and euthyroid dogs with non-thyroidal illness may fail to show an increase in total T4 concentrations after the exogenous TRH administration.
- A TSH assay has been developed for dogs that allowed the measurement of endogenous TSH after TRH administration. This advent made the TRH stimulation a more useful test.
- TRH stimulation test can differentiate secondary hypothyroidism (i.e. pituitary origin) from tertiary hypothyroidism (i.e. hypothalamic origin).
- If a dog has secondary hypothyroidism, the post-TRH TSH levels should be low to non-detectable.
- If a dog has tertiary hypothyroidism, the post –TRH TSH levels should be normal.
- Measurement of TSH after TRH administration can also be useful in hypothyroid cases in which serum endogenous TSH, fT4, or total T4 concentrations are non-diagnostic.
- An exaggerated TSH response to TRH should be expected in hypothyroid dogs with primary hypothyroidism.
- Preliminary studies showed that serum TSH peaks 20 minutes after 200 µg injection of TRH.
- Test protocol:
- Collect blood samples before and 6 hours after intravenous administration of 0.5 to 1 mg of TRH (Thyrel® TRH). A dose as low as 10 µg/kg appears to induce significant pituitary TSH stimulation with minimal side effects.
- Side effects:
- Cholinergic signs including defecation, vomiting, urination, and salivation are common for up to 30 minutes after TRH administration.
- TRH stimulation test – It is not accurate to diagnose primary hypothyroidism.
-
Important Facts
- The measurement of total T4 after the exogenous administration of TRH is not an accurate test to diagnose primary hypothyroidism.
- Normal dogs and euthyroid dogs with non-thyroidal illness may fail to show an increase in total T4 concentration after the exogenous TRH administration.
- The measurement of TSH after the exogenous administration of TRH can be used to diagnose primary, secondary, and tertiary hypothyroidism.
- If a dog has primary hypothyroidism, an exaggerated TSH response to TRH is expected.
- If a dog has pituitary (i.e. secondary) hypothyroidism, very low or no TSH response to TRH should occur.
- If a dog has hypothalamic (i.e. tertiary) hypothyroidism, a normal TSH response to TRH should be expected.
- Cholinergic signs including defecation, vomiting, urination, and salivation are common for up to 30 minutes after TRH administration.
-
-
- Thyroglobulin Autoantibody (TGAA) Test:
- This test is most valuable to diagnose subclinical or clinical lymphocytic thyroiditis.
- Keep in mind, a positive TGAA signifies that the patient has lymphocytic thyroiditis but not necessarily hypothyroidism. The reason for this is the slow developing nature of hypothyroidism, which requires at least 75% of both thyroid lobules to be affected before the glands become non-functional and clinical signs manifest.
- TGAA is a valuable test and should be performed early in life because lymphocytic thyroiditis is a genetic disorder and dogs with a positive TGAA test should not be bred.
- It has been reported that about 20% of dogs with positive TGAA will progress within one year to develop clinical or laboratory abnormalities compatible with hypothyroidism.
- Thyroglobulin Autoantibody (TGAA) Test:
-
Important Facts
- A positive TGAA test solely indicates the presence of lymphocytic thyroiditis.
- It may take months to years before a dog with positive TGAA manifests clinical signs of hypothyroidism.
- TGAA is a valuable test and should be performed early in life because lymphocytic thyroiditis is a genetic disorder and dogs with a positive TGAA test should not be bred.
-
-
- Therapeutic trial:
- It can be used as a diagnostic tool when test results are inconclusive (i.e. borderline low or low normal) and the patient has clinical signs compatible with hypothyroidism.
- Measure basal T4 concentrations prior to initiating a therapeutic trial.
- Be very critical when using a treatment trial to diagnose hypothyroidism!
- A 12-week period will allow sufficient time for resolution of all signs, including hair re-growth in most dogs, if hypothyroidism is present.
- Take the animal off thyroid supplementation if resolution or significant improvement of signs is not observed after 3 months of therapy and the 4 to 6 hours (peak concentration) post-pill basal T4 concentration is within the normal range or slightly above.
- Be aware if the pet makes “slight” improvement! Exogenously administered thyroid hormone can stimulate some hair growth even in dogs with non-thyroid illness.
- Therapeutic trial:
-
Important Facts
- Therapeutic trial can be used as a diagnostic tool.
- Be very critical when using a treatment trial to diagnose hypothyroidism!
- Discontinue the thyroid supplementation if resolution or significant improvement of signs is not observed after 3 months of therapy and the 4 to 6 hours (peak concentration) post-pill basal T4 concentration is within the normal range or slightly above.
- Be aware if the pet has some hair growth. Exogenously administered thyroid hormone can stimulate some hair growth even in dogs with non-thyroidal illness.
-
-
- Conclusion about the thyroid function tests:
- Currently, the best way to assess thyroid function in dogs is by measuring serum total T4 or fT4 and TSH on a single sample.
- The finding of a low total T4 or fT4 concentration with an elevated TSH concentration is diagnostic of hypothyroidism if the animal has a history and clinical signs suggestive of hypothyroidism.
- Remember, very few studies have been done to determine the effects of non-thyroid illness and medications on these diagnostic tests. Current findings indicate that T4 is more affected than fT4 by equilibrium dialysis and both are more affected than endogenous TSH.
- In a dog that may have concurrent non-thyroidal illness, measurement of serum fT4 by equilibrium dialysis and TSH is recommended. Ideally, however, you should not evaluate the thyroid function of dogs that are severely ill.
- Critical evaluation of serum TSH assays and measurement of fT4 by equilibrium dialysis as thyroid-function tests is necessary before we can say that the future is here.
- Remember, a therapeutic trial with L-thyroxine can be used to diagnose hypothyroidism but discontinue supplementation if clinical signs do not improve significantly or are not resolved after 12 weeks of therapy.
- A positive TGAA test does not necessarily indicate hypothyroidism but will indicate the presence of a hereditary disease (i.e. lymphocytic thyroiditis) and the dog should not be bred. Evaluate the thyroid function of a positive dog every 6 to 12 months to determine if she/he has developed hypothyroidism.
- Conclusion about the thyroid function tests:
-
-
Treatment
- Synthetic T4 (sodium levothyroxine):
- It is the treatment of choice.
- Dose: 0.02 mg/kg administered twice daily. Give it on an empty stomach (i.e. 2 hours before or after feeding) as food can reduce the bioavailability of L-thyroxine in dogs.
- Once-a-day administration can be tried after adequate clinical response is noted. However, a recent study showed that levothyroxine solution initially administered once daily controlled hypothyroidism in 85% of treated dogs.
- Modify the initial dose in aged dogs and dogs with diabetes mellitus, heart failure, renal and hepatic failures.
- Start with 25% of the standard dose.
- Increase dose by 25% every 2 to 4 weeks until the appropriate dose is reached (0.02 mg/kg twice daily).
- Monitoring response to therapy:
- Recheck the animal 6 to 12 weeks after initiation of therapy.
- Critically re-evaluate the clinical response:
- Lethargy and weakness should resolve in 7 to 10 days.
- Hair re-growth may take 12 weeks.
- Check post-pill T4 concentration at 4 to 6 hours (peak serum T4 concentration) after morning medication when administering the drug twice daily. Check post-pill T4 levels at 24 hours (before the daily dose = trough serum T4 concentration) when administering the drug once daily.
- Post-pill T4 values should be at or slightly above the upper limit of the reference range when administering the levothyroxine twice daily and at any point within the normal range when administering the drug once daily.
- Synthetic T4 (sodium levothyroxine):
Important Facts
- Synthetic T4 is the treatment of choice at the dose of 0.02 mg/kg given twice daily.
- Modify the initial dose regimen in aged dogs and dogs with diabetes mellitus, heart failure, renal and hepatic failures.
- Recheck the animal 6 to 12 weeks after initiation of therapy and critically re-evaluate response to therapy: lethargy and weakness should resolve in 7 to 10 days; hair re-growth may take 12 weeks.
- Check post-pill T4 concentration at 4 to 6 hours (peak serum T4 concentration) after morning medication when administering the drug twice daily. Check post-pill T4 concentration at 24 hours (before the daily dose = trough serum T4 concentration) when administering the drug once daily.
- Post-pill T4 value should be at or slightly above the upper limit of the reference range when administering the levothyroxine twice daily and at any point within the normal range when administering the drug once daily.
References
Bolton TA & Panciera DL. Influence of medications on thyroid function in dogs: An update. J Vet Intern Med 2023; 1-15.
Bugbee A, Rucinsky R, Cazabon S et al. 2023 AAHA selected endocrinopathies of dogs and cats guidelines. J Am Anim Hosp Assoc 2023; 59:113-135.
Feldman E.C. & Nelson R.W. 1996. Hypothyroidism. In: Canine and Feline Endocrinology and Reproduction. 3rd ed. Philadelphia: W.B. Saunders Co, 2003; 88-151.
Ferguson DC. Testing for hypothyroidism in dogs. Vet Clin Small Anim 2007; 37: 647-69.
Graham PA, Lundquist RB, Refsal KR et al. A 12-month prospective study of 234 thyroglobulin antibody positive dogs which had no laboratory evidence of thyroid dysfunction. J Vet Intern Med 2001; 14:298.
Graham PA, Refsal KR and Nachreiner RF. Etiopathologic findings of canine hypothyroidism. Vet Clin Small Anim 2007; 37:617-631.
Lathan P. Laboratory diagnosis of thyroid and adrenal disease. Vet Clin Small Anim 2023; 53:207-224
Le Traon G, Bugaud S, Horspool LJ. Pharmacokinetics of total thyroxine in dogs after administration of an oral solution of levothyroxine sodium. J Vet Pharmacol Ther 2008; 31:95-101.
Mooney CT. Canine hypothyroidism: A review of aetiology and diagnosis. New Zealand Vet J 2011; 59:105-114.
Panciera DL. Clinical Manifestations of canine hypothyroidism. Vet Med 1997; 44-49.
Panciera DL. Thyroid-function testing: Is the future here? Vet Med 1997; 50-57.
Panciera DL. Treating hypothyroidism. Vet Med 1997; 58-68.
Scott-Moncrieff JC. Clinical signs and concurrent diseases of hypothyroidism in dogs and cats. Vet Clin Small Anim 2007; 37: 709-722.
Soler Arias EA, Castillo VA, Garcia JD et al. Congenital dyshormonogenic hypothyroidism with goiter caused by a sodium/iodide symporter (SLC5A5) mutation in a family of Shih-Tzu dogs. Domest Anim Endocrinol 2018; 65:1-8.

