2.13 Mucous Membrane Pemphigoid – Dogs and Cats
-
General Considerations
- Mucous membrane pemphigoid (MMP), also referred to as cicatricial pemphigoid, is a rare subepidermal blistering autoimmune disease reported in dogs and cats.
- It is the most common autoimmune subepidermal blistering disease of dogs accounting for about 48% of the cases.
Important Facts
- Mucous membrane pemphigoid is a rare subepidermal blistering autoimmune disease reported in dogs and cats.
- It is the most common autoimmune subepidermal blistering disease of dogs.
-
Pathogenesis
- Autoantibodies (mostly IgG) are generally directed against a component of the basement membrane known as the NC16A domain of collagen XVII. Specifically, the main targeted basement membrane antigen reported is BPAG1 or BPAG2, but other antigens of the collagen XVII such as laminin 332 (5) and the C-terminus region or combinations may be seen.
Important Facts
- Autoantibodies (mostly IgG) are generally directed against a component of the basement membrane known as the NC16A domain of collagen XVII.
-
Clinical Signs: The information was based on a comprehensive review on autoimmune subepidermal blistering diseases in animals.
-
- Signalment:
- The German shepherd dog and its crosses appear to be most affected, representing about one third of the reported cases.
- There is no sex predilection.
- The reported age at disease onset range from 1 to 15 years (median 5 years). However, one third of the dogs are at least 8 years old at the time of disease onset.
- Lesions:
- Vesicles (blisters) and bullae are initially formed; however, they are transient and rarely seen.
- Ruptured vesicles and bullae progress to deep erosions and/or ulcers and crusts. Hypopigmentation and scarring can be seen in chronic cases.
- Signalment:

-
-
- Pain, lethargy, ptyalism, and halitosis will be present in severe cases.
- Pruritus is uncommon.
- Distribution:
- Oral cavity is the most commonly affected body region in the dog and is reported in 68% of the cases. Gingiva and palate are the sites more often affected within the oral cavity.
-

-
-
- Other commonly affected sites in the dog include mucocutaneous junctions such as, eyelids/periocular areas, nose and around the nose, labial/perilabial areas, and perianal/perigenital areas. The concave aspect of the pinnae can also be affected.
-

Courtesy of Thierry Olivry, case material NCSU.

Courtesy of Thierry Olivry, case material NCSU.
-
-
- Bilateral symmetry of lesions are quite common.
- Haired skin away from mucosae (e.g. elbow, groin, axilla, interdigital, periungual, scrotum) are uncommonly affected.
- Only four cases have been reported in cats.
- The age at disease onset ranged from 1 to 7 years.
- All four cats developed vesicles and/or deep erosions or ulcers at mucosal and mucocutaneous sites.
- The lips and oral cavity were the areas more often affected but lesions also developed on the nasal planum, eyelids, conjunctivae, and concave pinnae.
-
Important Facts
- German shepherd dogs and their crosses appear to be predisposed.
- Males and females are equally affected in dogs.
- The median age at disease onset in dogs is 5 years, but one third of the dogs are at least 8 years old at disease onset.
- Primary (vesicles, bullae) and/or secondary (erosions, ulcers, crusts, hypopigmentation, and scarring) lesions are present at the oral mucosa (most frequently) and/or mucocutaneous regions (lips, eyes, perinasal, perianal, and genitalia).
- Lesions are usually symmetrical and generally spares non-mucosae and non-mucocutaneous areas, and the pads.
- Lesions were similar in the four reported cases in cats but, interestingly, they only developed on the head with the oral mucosal and the lips being more often affected.
- Pain, lethargy, and ptyalism can be present in severe cases.
-
Diagnosis
- Differential diagnoses:
- All diseases that cause predominantly vesicles and deep erosions and ulcers at the oral mucosa including mucocutaneous lupus erythematosus, bullous pemphigoid, epidermolysis bullosa acquisita, erythema multiforme major, pemphigus vulgaris, toxic epidermal necrolysis, drug reaction, and oral variants of cutaneous epitheliotropic lymphoma.
- A compatible history and characteristic clinical signs are important parts of the diagnostic equation.
- Cytology:
- Direct smears prepared from the exudate collected from intact vesicles or bullae or from the exudate obtained from an ulcer, erosion, or underneath a crust will not reveal acantholytic keratinocytes.
- This test is not diagnostic but is important to investigate the presence of secondary infections.
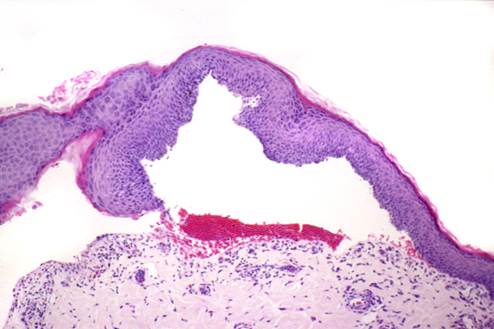
- Histopathology:
- Subepidermal or submucosal cleft and vesicle formation with little or no inflammatory infiltrate. Superficial dermis, especially at affected mucosal sites, show a lymphoplasmacytic band-like infiltrate.
- Depending on the pathologist and biopsy samples, the diagnosis may not be apparent.
- Biopsy an intact vesicle/bulla if possible; otherwise, sample the active border of an erosion or ulceration.
- Aim to submit the biopsy samples to a pathologist with interest in dermatohistopatholgy. Make sure to include a detailed history and clinical signs description. If possible, also submit good quality photos.
- Ask the pathologist to perform periodic-acid Schiff (PAS) staining of the sample or immunohistochemistry for collagen IV. The PAS stain will color the lamina densa of the basement membrane zone magenta. In the case of mucous membrane pemphigoid, the floor of the vesicle/bulla should stain. This test will help differentiate mucous membrane pemphigoid from epidermolysis bullosa acquisita cases. Keep in mind that the sensitivity of this test is low.
- Depending on the pathologist and biopsy samples, the diagnosis may not be apparent.
- Subepidermal or submucosal cleft and vesicle formation with little or no inflammatory infiltrate. Superficial dermis, especially at affected mucosal sites, show a lymphoplasmacytic band-like infiltrate.
- Differential diagnoses:
Courtesy of Thierry Olivry, case material NCSU.
-
- Direct immunofluorescence and immunohistochemistry -These tests detect autoantibodies (typically IgG) bound to the basement membrane zone of the skin and mucosa:
- Commercial laboratories do not perform these tests routinely.
- Staining shows linear deposition of immunoglobulins along the basement membrane zone.
- Remember! Skin biopsy is submitted for this test (samples should be fixed in Michel’s fixative for immunofluorescence and formalin for immunohistochemistry).
- Positive in about 93% of the canine reported cases.
- Indirect immunofluorescence:
- Best results with salt-split canine gingiva as substrate – It is positive in 77% of canine reported cases.
- Most commonly, split is present in the epidermal side of the split (i.e. roof), but may be seen in both sides of the split or in the dermal side in some cases (i.e. floor).
- Serum sample is used for this test.
- CBC, chemistry profile, urinalysis:
- Findings are non-specific. These tests are used as baseline for monitoring potential side effects associated with therapy.
- Direct immunofluorescence and immunohistochemistry -These tests detect autoantibodies (typically IgG) bound to the basement membrane zone of the skin and mucosa:
Important Facts
- Thorough history and characteristic clinical signs are important diagnostic information.
- Histopathology is the most important diagnostic test and reveals a subepidermal cleft and vesicle formation with little to no inflammatory infiltrate in the vesicle. Moreover, a lymphoplasmacytic band-like infiltrate in the superficial dermis at affected mucosal sites is typically present.
- Direct immunofluorescence using salt-split canine gingiva is positive in 93% of the cases; however, it is not available for routine use in clinical practice.
- Indirect immunofluorescence tests are not frequently used as a diagnostic tool because false negative results often occur.
-
Treatment
- One or more of the following options is recommended: (See “Therapy for Autoimmune Diseases” for dose and specifics on treatment regimens).
- Glucocorticoids – Typically effective if used in combination with another immunomodulatory drug.
- Azathioprine – Do not use it in cats because they develop bone marrow suppression.
- Cyclosporine.
- Mycophenolate mofetil.
- Chlorambucil.
- Doxycycline and niacinamide. Try to avoid this treatment modality to prevent bacterial resistance to antibiotics (practice antibiotic stewardship).
- Dapsone.
- Discontinuation of therapy has resulted in disease recurrence.
- Prognosis:
- The prognosis is good to guarded. Complete remission has been reported in most cases with various treatment regimens.
- One or more of the following options is recommended: (See “Therapy for Autoimmune Diseases” for dose and specifics on treatment regimens).
References
Bizikova P, Linder KE, Anderson JG. Erosive and ulcerative stomatitis in dogs and cats: which immune-mediated diseases to consider? J Am Vet Med Assoc 2023; doi.org/10.2460/javma.22.12.0573.
Bizikova P, Olivry T, Linder K et al. Spontaneous autoimmune subepidermal blistering diseases in animals: a comprehensive review. BMC Vet Res 2023; https://doi.org/10.1186/s12917-023-03597-1.
Medleau L, Hnilica KA. Chapter 8. Autoimmune and immune-mediated skin disorders. In: Small Animal Dermatology: A color Atlas and Therapeutic Guide 2006. 2nd ed. W.B. Saunders, Missouri, 189-227.
Miller, Griffin and Campbell. Chapter 9. Autoimmune and immune-mediated dermatoses. In: Muller & Kirk’s Small Animal Dermatology 2013. 7th ed., W.B. Saunders, Missouri; 432-462.
Olivry T. Auto-immune skin disease in animals: time to reclassify and review after 40 years. BMC Vet Res 2018; https://doi.org/10.1186/s12917-018-1477-1.
Olivry T, Chan LS. Autoimmune blistering dermatoses in domestic animals. Clin Dermatol 2001; 19(6):750-760.
Olivry T., Jackson HA. Diagnosing new autoimmune blistering skin diseases of dogs and cats. Clin Tech Small Anim Pract 2001; 16: 225-229.

