2.7 Facial Discoid Lupus Erythematosus – Dogs
-
General Considerations
- Facial discoid lupus erythematosus also referred as discoid or cutaneous lupus erythematosus, is the second most common autoimmune skin disease reported in dogs, after pemphigus foliaceus.
- It is rarely reported in cats.
- facial discoid lupus erythematosus is a relatively benign nasal planum-predominant skin disease with no systemic signs.
- Canine breeds commonly affected include collies, Shetland sheepdogs, German shepherd dogs, and Siberian huskies.
Important Facts
- Facial discoid lupus erythematosus is the second most common autoimmune skin disease in dogs, after pemphigus foliaceus. It is rarely reported in cats.
- Dogs are usually healthy with only skin involvement.
-
Clinical Signs
- Signalment: The information is based on a comprehensive review article on cutaneous lupus erythematosus in dogs.
- German shepherd dogs and their crosses accounted for 32/104 (31%) of the cases.
- Reported age of onset range from 1 to 12 years (median: 7 years).
- The female/male ratio is 0.7.
- Lesions:
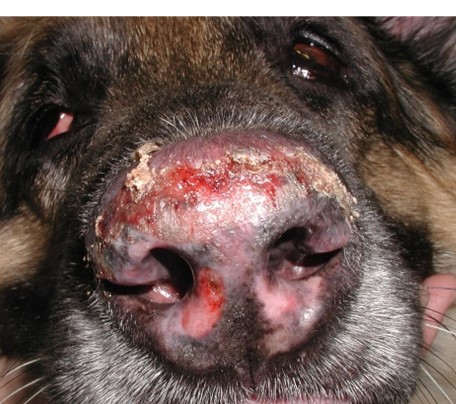
- Lesions usually start as depigmentation, erythema, and scaling of the nasal planum and progress to deep erosions or shallow ulcers, crusts and loss of architecture of the nasal planum skin in chronic cases.
- Signalment: The information is based on a comprehensive review article on cutaneous lupus erythematosus in dogs.

-
-
- Lesions usually heal with atrophic and sometimes disfiguring scars characterized by depigmentation and loss of normal cobblestone architecture of the nose.
-

-
-
- Lesions are exacerbated by sunlight because the skin pigment is lost.
-

-
- Lesion distribution:
- Lesions are most often limited to the nasal planum.
- Lesion distribution:


-
-
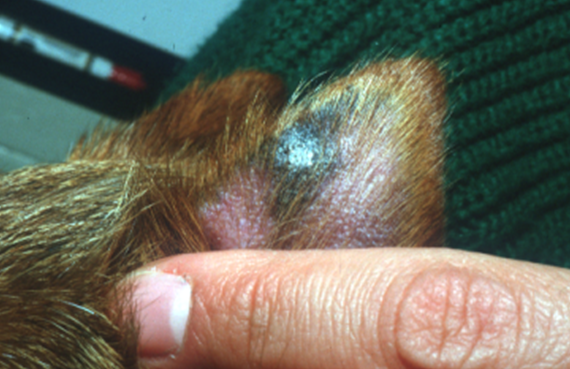
- Other body regions that are less commonly affected include the dorsal-proximal muzzle, periocular skin, pinnae, and lips.
-


Important Facts
- The nasal planum is affected in all cases but some dogs can also develop lesions on the dorsal-proximal muzzle, pinnae, lips, and periocular areas.
- Depigmentation, erythema, and scaling are the initial lesions. Lesions evolve to deep erosions or shallow ulcers, crusting, and eventually loss of normal cobblestone appearance of the nasal planum.
- Deep erosive or ulcerative lesions will heal with scar.
- Lesions are exacerbated by sunlight.
-
Diagnosis
- Differential diagnoses:
- Pemphigus foliaceus, pemphigus erythematosus, mucocutaneous pyoderma, uveodermatological syndrome, and epitheliotropic T cell lymphoma.
- Characteristic history and clinical signs are important parts of the diagnosis equation.
- Cytology:
- Acantholytic cells are not present. This helps differentiate facial discoid lupus erythematosus from pemphigus foliaceus and pemphigus erythematosus.
- Evidence of a secondary bacterial infection is common.
- Histopathology:
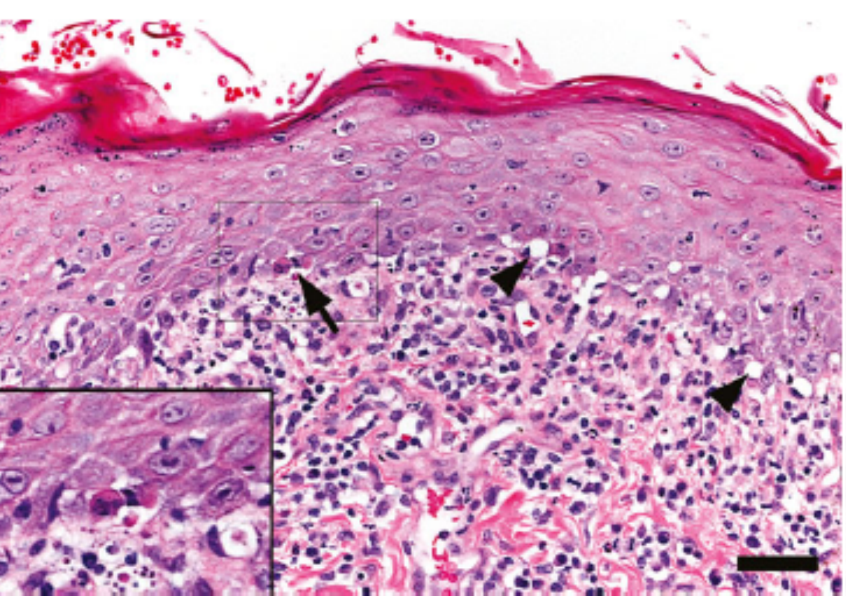
- Interface dermatitis reaction characterized by hydropic-vacuolar changes at the basement membrane zone and basal cell layer and lichenoid band-like infiltrate at the dermal-epidermal junction consisting primarily of lymphocytes and plasma cells. The lichenoid band-like infiltrate at the dermal-epidermal junction can be seen with other inflammatory disease of the nasal planum. Individual apoptotic keratinocytes in the lower epidermis and pigmentary incontinence are additional findings.
- Differential diagnoses:
Source: Olivry T et al, Vet Derm 2015; 26:256-255.
-
-
- Select non-ulcerated depigmented macules to biopsy.
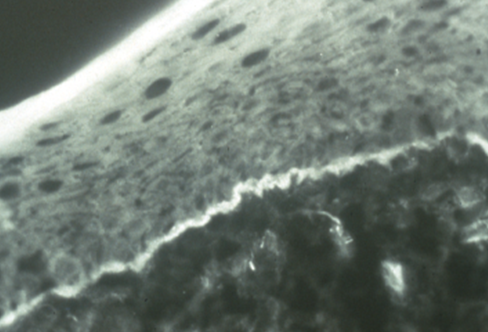
- Direct immunofluorescence or immunohistochemistry:
- Deposition of immunoglobulin or complement at the basement membrane zone resulting in fluorescence or peroxidase reaction at the dermal-epidermal junction.
- Remember! Do not rule out facial discoid lupus erythematosus if the results are negative.
- History, clinical signs, and histopathologic findings are more valuable diagnostic tools.
- Preserve samples in Michel’s solution for immunofluorescence and formalin for immunohistochemistry.
-
-
- Antinuclear antibody (ANA) test:
- Negative or very low titers. This is not a useful test for the diagnosis of facial discoid lupus erythematosus.
- Antinuclear antibody (ANA) test:
Important Facts
- Characteristic history (i.e. the dog developed lesions on the nasal planum that gets worse under the sunlight but the animal is feeling well overall) and typical clinical signs (i.e. depigmentation, erythema, scaling. then erosions/ulcers, and crusts on nasal planum) are important information for a definitive diagnosis.
- Histopathology is essential for a definitive diagnosis and it will show hydropic degeneration of the basal cell layer and individual apoptotic keratinocytes. A lichenoid band-like inflammatory infiltrate at the dermal-epidermal junction will be also present but this finding is not specific for facial discoid lupus erythematosus and will likely be present in other inflammatory diseases of the nasal planum or mucosal sites.
- Direct immunofluorescence or immunohistochemistry will show deposition of immunoglobulin and/or complement at the dermal-epidermal junction. Remember! False positive results are common.
- Antinuclear antibody (ANA) test is negative or yield very low titers.
-
Treatment
- Prognosis is usually good with appropriate therapy.
- Treatment has to be individualized due to the wide spectrum of clinical presentation among the animals.
- One or more of the following are treatment options for facial discoid lupus erythematosus: (See below “Therapy for Autoimmune Diseases” for dose or specifics on treatment regimens).
- Glucocorticoids – Oral and/or topical.
- Cyclosporine or topical tacrolimus (Protopic® ointment 0.1% or 0.03%).
- Oclacitinib (Apoquel®) – Anecdotal reports have shown its good efficacy in treating facial discoid lupus erythematosus.
- A tetracycline (i.e. tetracycline, doxycycline, minocycline) and niacinamide. Try to avoid this treatment modality to prevent bacterial resistance to antibiotics (practice antibiotic stewardship).
- Azathioprine – May be used in dogs for the treatment of refractory cases.
- Sunscreen – Important to protect against sun damage.
References
Medleau L, Hnilica KA. Chapter 8. Autoimmune and immune-mediated skin disorders. In: Small Animal Dermatology: A color Atlas and Therapeutic Guide 2006. 2nd ed. W.B. Saunders, Missouri, 189-227.
Miller, Griffin and Campbell. Chapter 9. Autoimmune and immune-mediated dermatoses. In: Muller & Kirk’s Small Animal Dermatology 2013. 7th ed., W.B. Saunders, Missouri; 432-462.
Olivry T. Auto-immune skin disease in animals: time to reclassify and review after 40 years. BMC Vet Res 2018; https://doi.org/10.1186/s12917-018-1477-1.
Olivry T, Chan LS. Autoimmune blistering dermatoses in domestic animals. Clin Dermatol 2001; 19(6):750-760.
Olivry T, Linder KE, Banovic F. Cutaneous lupus erythematosus in dogs: a comprehensive review. BMC Vet Res 2018; https://doi.org/10.1186/s12917-018-1446-8.

