4.5 Systemic Mycosis – Cryptococcosis – Small Animals
Learning Objectives
- Remember! Cryptococcus neoformans is a yeast-like fungus, which contains a large mucinous capsule. It is most frequently associated with pigeon droppings or decaying plant materials in hollow of trees.
- Know that the organism after inhaled into the upper or, less commonly, lower respiratory tract can disseminate via blood. Infection can extent directly from the respiratory tract to the CNS and eyes.
- Know that cryptococcosis is the most common systemic mycosis of cats. Cats often will present with upper respiratory lesions characterized by a flesh-colored polyp-like lesion inside the nostril or a firm to mushy subcutaneous mass over the dorsal aspect of the muzzle. CNS, ocular and skin signs can also be present. Describe the clinical signs in dogs.
- Know how to diagnose this disease. Remember! The latex agglutination test (capsular antigen test) can be used not only to diagnose the disease but also to monitor response to treatment. It can be falsely negative if only the skin is affected.
- Know how to manage cryptococcosis. Remember to prescribe fluconazole if the CNS is involved since it penetrates the blood brain barrier.
- Remember that treatment should be continued until the latex agglutination test becomes negative.
- Learn the disease prognosis to be able to discuss it with your client.
-
General Considerations:
- The establishment and spread of infection are highly dependent on host immunity. However, underlying diseases are often not detected in dogs and cats with cryptococcosis.
- Cryptococcosis in dogs and cats is accelerated or worsened by glucocorticoid therapy.
Important Facts
- Cryptococcosis in dogs and cats is accelerated or worsened by glucocorticoid therapy.
-
Etiology and Pathogenesis:
- Cryptococcosis is caused by Cryptococcus (C) neoformans and C. gattii.
- Cryptococcus spp. is a dimorphic fungus presenting as filamentous organisms in the environment and yeast in body tissues.
- The yeast measures 2 – 5 µm in diameter and has a heteropolysaccharide capsule (1 – 30 µm).
-
- The exact mode of infection is unknown:
- Inhaled organisms lodge primarily in the upper respiratory tract and can extent to the central nervous system via the cribriform plate and olfactory bulb and tract resulting in meningoencephalitis.
- The infection may also spread to the optic nerve due to anatomical proximity causing optic neuritis.
- The infection may disseminate via blood to become systemic.
- Less commonly, the inhaled organisms lodge into the lower respiratory tract and from there the infection may disseminate via blood to become systemic.
- Cellular immune response is important in preventing or eliminating the infection.
- Infection can develop in immunosuppressed and immunocompetent animals.
- Inhaled organisms lodge primarily in the upper respiratory tract and can extent to the central nervous system via the cribriform plate and olfactory bulb and tract resulting in meningoencephalitis.
- The exact mode of infection is unknown:
Important Facts
- Cryptococcus neoformans is a yeast-like fungus in body tissues and measures 2–5µm in diameter. It has a heteropolysaccharide capsule 1–30µm thick.
- Inhaled organisms lodge primarily in the upper respiratory tract and from there they can extend to the central nervous system and ocular system.
- Organisms inhaled into the upper or lower respiratory tract can disseminate via blood to become systemic.
-
Geographic Distribution:
- C. neoformans is found worldwide and C. gattii distribution is restricted to tropical and subtropical climates (USA [Washington State, Oregon, California], Canada [British Columbia], Australia, parts of Latin America, New Guinea, Southeast Asia, and Central Africa).
-
Natural Reservoir and Epidemiology:
- In Australia, C. gattii is associated with dead plant material in hollows of eucalyptus trees. In British Columbia, Canada, it is associated with live tree bark.
- C. neoformans organisms are associated with weathered bird droppings (especially pigeons), and decaying plant material in hollows of certain trees. It can remain viable in pigeon droppings for at least 2 years unless exposed to drying conditions and sunlight.


Important Facts
- Cryptococcus neoformans is primarily associated with weathered pigeon droppings.
- Cryptococcus gattii is associated with live tree bark or decaying plant material in hollows of eucalyptus or other trees.
-
Clinical Signs
- Cats:
- It is the most frequent systemic mycosis reported in cats.
- There are no sex, age and breed predilections.
- Upper respiratory infection occurs in about 80% of the cases and is characterized by sneezing, snuffing and unilateral or bilateral mucopurulent, serous or hemorrhagic discharge.
- In about 70% of the cases, a flesh-colored, polyp-like mass is visible in the nostril, or a firm to mushy subcutaneous swelling over the bridge of the nose is evident.
- Submandibular lymphadenomegaly is common.
- Cats:

-
-
- Lower respiratory signs are rare.
- Central nervous system and ocular signs may be present, but are rare in cats (~15-25%).
- Ocular signs usually indicates central nervous system involvement.
-

-
-
- Skin and subcutaneous tissues are involved in about 40% to 50% of the cases. Lesions include nodules, cold abscesses, draining tracts and ulcerations.
-

-
-
- Lymphadenomegaly and weight loss can be seen.
-
Important Facts
- Cryptococcosis is the most frequent systemic mycosis reported in cats.
- In about 70% of the cases, a flesh-colored, polyp-like mass is visible in the nostril(s), or a firm to mushy subcutaneous swelling on the dorsal aspect of the muzzle is evident.
- Central nervous system and ocular signs may occur and they are often an extension of the nasal cavity infection but may also occur via hematogenous dissemination.
- Skin nodules, draining tracts and abscesses occur in about 40% to 50% of the cases.
- Lymphadenomegaly and weight loss can be seen.
-
- Dogs:
- Young adult dogs (3-4 years) and large breeds are predisposed.
- Skin lesions develop in about 25% of the dogs. They are characterized by ulcers in the nose, tongue, gums, hard palate and nail folds.
- Dogs:

-
-
- Dogs with C. neoformans infection usually has disseminated disease characterized by fever, respiratory signs, vomiting, diarrhea, lameness, lymphadenomegaly, central nervous system sings and ocular signs. A report described a case of intestinal cryptococcosis in a dog.
-
Important Facts
- Young dogs and large breeds are predisposed.
- Disseminated disease occurs more often in dogs infected with C. neoformans.
-
- Differential diagnoses:
- Deep pyoderma.
- Sporotrichosis.
- Mycobacterial (atypical mycobacterial) granuloma.
- Foreign body granuloma.
- Opportunistic fungal or bacterial (Actinomyces, Nocardia) infections.
- Sterile pyogranuloma.
- Neoplasia.
- Differential diagnoses:
-
Diagnosis
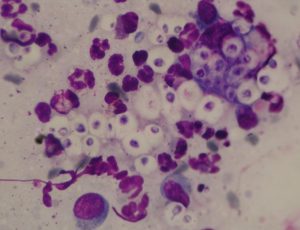
- Cytological examination of samples from the nasal and skin exudates, masses, cerebrospinal fluid (CSF), and ocular fluid has revealed organisms in most cases. Special stain with India ink, new methylene blue or Gram’s stain helps visualizing the organisms. Cytology should show budding yeasts with large mucinous capsules.
- Biopsy shows a pyogranulomatous inflammation (i.e. neutrophils and macrophages) surrounding budding yeasts with a large mucinous capsule. If routine H&E stain does not show the organisms, request the following special stains: Mayer’s mucicarmine, which stain the capsule red, PAS, and GMS stains. To learn about the characteristic of the yeast in histology refer to the review article by Hoffmann et al, 2023.
- The only useful serologic test is a latex agglutination test that detects cryptococcal capsular antigen.
- The sensitivity ranges from 90% to 100% and the specificity from 97% to 100%. This test is more sensitive in cats than dogs.
- This test can also be performed with serum and CSF fluid samples.
- A positive titer is > 1/200. It may be negative in cats with disease localized solely to the skin.
- The test may also be used to monitor response to therapy. Use the same methodology during monitoring because titer results can differ significantly between different kits.
- This test can also be performed with CSF and urine samples.
- Culture should be done whenever possible. It specifies the agent and allows for performance of susceptibility tests. Sabouraud’s agar without cycloheximide or Birdseed agar. Birdseed agar can distinguish Cryptococcus spp. organisms from other fungi by the brown-color effect in the agar.
Important Facts
- History and clinical signs are important diagnostic tools.
- Cytology of samples collected from nose and skin exudates, masses, and cerebrospinal and ocular fluids.
- Biopsy should show budding yeasts with a large mucinous capsule associated with a pyogranulomatous inflammation.
- Fungal culture should be attempted whenever possible.
- A latex agglutination test, which detects fungal capsular antigen, can be used as a diagnostic test and to monitor response to therapy. Remember to use the same laboratory/methodology during monitoring because the kits can differ significantly.
-
Treatment
- Itraconazole:
- Dose:
- It is currently the drug of choice to treat cats.
- Dogs and cats: 5 mg/kg q 12-24h.
- Cats: 5-10 mg/kg q 24 h if capsules; 3-5 mg/kg q 24 h if oral suspension.
- The oral suspension containing cyclodextrin has greater bioavailability than the capsule formulation.
- Itraconazole has been used successfully to treat Cryptococcus meningitis.
- Monitor liver enzymes during treatment.
- Dose:
- Fluconazole: Good if central nervous system and ocular signs are present. Use the same dose protocol to treat blastomycosis.
- Amphotericin B: deoxycholate or lipid complex (Abelcet®).
- Good option for severe cases with central nervous system involvement.
- Dose:
- Dogs: 0.5 mg/kg IV q 48h. Cumulative dose: 5-10 mg/kg
- Cats: 0.25 mg/kg IV q 48h. Cumulative dose: 4-8 mg/kg
- Combine with 5-flucytosine (250 mg orally q 8h) in disseminated cases and cases involving the central nervous system as it has good blood-brain-barrier penetration. Only use in cats because dogs often have a severe reaction to fluocytosine (i.e. malaise, fever, facial pruritus, mucocutaneous ulceration).
- Ketoconazole:
- Dogs: 5 to 10 mg/kg q 12-24 h. Avoid or use carefully in cats because they do not tolerate it.
- Less efficacious than itraconazole.
- Monitor liver enzymes during treatment.
- Terbinafine:
- A report described the efficacy of using terbinafine at 30 mg/kg per day, orally, to treat intestinal cryptococcosis in a dog after surgical excision of the affected area. This case was previously treated with itraconazole and lipid-complexed amphoterin B but the disease relapsed after a short remission (cryptococcal antigen titer decreased but never resolved).
- Posaconazole and Voriconazole.
- Posaconazole is a newer triazole structurally related to itraconazole.
- Dose:
- Dogs: 5-10 mg/kg q 12-24h. Cats: 5 mg/kg q 24h.
- Side effects:
- Inappetence, vomiting, diarrhea and increase in liver enzymes.
- Monitor liver enzymes during treatment.
- Voriconazole is a newer triazole structurally related to fluconazole.
- Dose:
- Dogs: 4-5 mg/kg q 12h. Cats: 2.68 to 5.10 mg/kg q 72-96h or 12.5 mg/cat q 72h. The dose for unusually large or small cats should be based in mg/kg and not mg/cat. At this dose regimen, the reported side effects include hyporexia, weight loss, and less commonly ALT increase.
- Cats treated with voriconazole at the dose range of 4.32 mg/kg to 13 mg/kg q 24h are prone to develop various side effects that include one or more of the following: inappetence, mydriasis, apparent blindness, ataxia, nystagmus, tremors, pelvic limb paralysis, cutaneous drug reaction, azotemia, decreased menace and decreased pupillary reflexes.
- Monitor liver enzymes during treatment.
- Excise granuloma lesions if feasible.
- Treat for at least 30 days after resolution of clinical signs and a negative latex agglutination test is obtained.
- Cryptococcosis can be more difficult to manage in dogs than in cats.
- Itraconazole:
Important Facts
- Itraconazole is currently the drug of choice for cats.
- Prescribe fluconazole if CNS is involved.
- Surgically remove granuloma lesions.
- Treat for at least 30 days after resolution of clinical signs and a negative latex agglutination test is obtained.
-
Prognosis
- Good if only nasal or cutaneous disease.
- Poor with meningoencephalitis.
- Use capsular antigen test to monitor the disease and to decide when to stop therapy.
Important Facts
- Prognosis is poor if meningoencephalitis is present.
- Use capsular antigen test to monitor response to therapy.
- Treat for at least 30 days after after resolution of clinical signs and a negative latex agglutination test is obtained.
References
Barrs VR, Bęczkowski PM, Talbot JT et al. Invasive fungal infections and oomycoses in cats. 1. Diagnostic approach. J Fel Med Surg 2024; doI: 10.1177/1098612X231219696
Barrs VR, Hobi S, Wong A et al. Invasive fungal infections and oomycoses in cats. 2. Antifungal therapy. J Fel Med Surg 2024; doI: 10.1177/1098612X231220047
Easterwood LF, Harkin KR, Rankin AJ. Oral voriconazole therapy in cats with histoplasmosis yielded mild side effects and a favorable outcome. J Am Vet Med Assoc 2023; doi.org/10.2460/javma.23.05.0276.
Greene CE. Infectious Diseases of the Dog and Cat. 4th ed. St. Louis, Missouri, Elsevier, Saunders, 2012.
Hoffmann AR, Ramos MG, Walker RT et al. Hyphae, pseudohyphae, yeasts, spherules, spores, and more: A review on the morphology and pathology of fungal and oomycete infections in the skin of domestic animals. Vet Pathol 2023; doi.org/10.1177/03009858231173715
Olsen GL, Deitz KL, Flaherty HA et al. Use of terbinafine in the treatment protocol of intestinal Cryptococcus neoformans in a dog. J Am Anim Hosp Assoc 2012; 48:3, 216-220.
Rippon JW. Medical Mycology. Philadelphia, WB Saunders, 1988.
Miller WH, Griffin CE, Campbell KL. Muller & Kirk’s Small Animal Dermatology. 7th ed. St. Louis, Missouri, Elsevier, Mosby, 2013.
Vishkautsan P, Papich MG, Thompson GR III et al. Pharmacokinetics of voriconazole after intravenous and oral administration to healthy cats. Am J Vet Res 2016; 77: 931–939.

