4.7 Systemic Mycosis – Coccidioidomycosis – Small Animals
Learning Objectives
- Know that Coccidioides spp. is a dimorphic soil fungus, which lives in the body as endospores inside large spherules. Know also that it likes sandy, alkaline soil, high environmental temperatures and low rainfall regions. Geographically this area includes Southwestern U.S., Northern Mexico, and Central and South America.
- Know that most infections occur through inhalation of fungal arthrospores into the lungs and dissemination via the blood and lymphatics to become systemic. Primary cutaneous inoculation can also occur but it is rare.
- Know how the disease manifests clinically in dogs and cats.
- Know that history and clinical signs are important diagnostic tools. Cytology of exudate and biopsy will show a pyogranulomatous infiltrate with or without spherules with endospores (sensitivity of cytology and histopathology is low).
- Know that serologic tests for IgM and IgG antibody have good sensitivity and specificity.
- Know the treatment and disease prognosis. Remember to treat this disease for at least 30 days past clinical resolution of signs and an antibody titer ≤ 1:2.
-
Etiology and Pathogenesis
- Coccidioidomycosis is caused by Coccidioides immitis (San Joaquin valley – California) and Coccidioides posadasii (worldwide).
- It is a dimorphic soil fungus.
- Dimorphism:
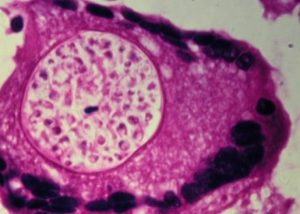
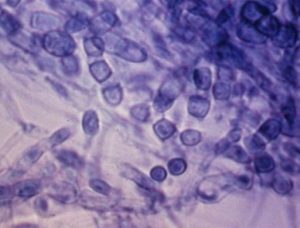
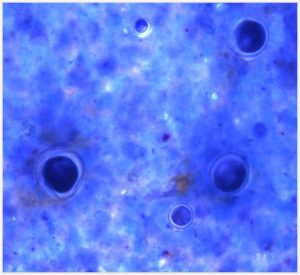
- When exposed to the body temperature the fungal converts to a yeast form. It forms a spherule that when mature acquires the size of 20 – 200 µm in diameter. The spherule carries 200 to 300 endospores.
-
-
- In the soil, the fungus has a filamentous form known as mycelium.
-
-
- The fungus arthrospores are inhaled into the lungs and disseminated via blood and lymphatic to become systemic.
- Primary cutaneous inoculation can occur but it is rare.
Important Facts
- Coccidioides immitis is a dimorphic saprophytic fungus.
- The organisms live in the body as spherules containing endospores and in the soil as mycelium.
- Most infections occur by inhalation into the lung of fungal elements, which disseminate via blood and lymphatic to become systemic.
- Primary cutaneous inoculation occurs rarely.
-
Geographic Distribution
- Southwestern U.S.A (California, Texas, Arizona, New Mexico, Nevada, Utah), Northern Mexico, and Central and South America such as Colombia, Guatemala, Honduras, Venezuela, Northeastern Brazil, Argentina, Paraguay, and Bolivia.
-
Natural reservoir and epidemiology
- The ecologic niche of the fungus is characterized by semiarid to arid, sandy-alkaline soil, high environmental temperature, low rainfall and low elevations above sea level.
- Serologic surveys indicate that most human and canine inhabitants of endemic areas become infected.
-
Pathogenesis
- Infection typically occurs after a period of moist conditions needed for the fungus to grow in the soil, followed by a period of dry environment and soil disruption such as earthquakes, construction, heavy rainfall etc.
- After inhalation, the arthroconidia transforms in spherules, which will mature to develop hundreds of endospores. Eventually, the spherule wall will break causing the release of the endospores. Neutrophils and macrophages are brought to the site leading to a pyogranulomatous response. In animals that are unable to mount an immune response and contain or eliminate the organisms, the endospores will disseminate to the lymphatics, tracheobronchial lymph nodes and hematogenously to various organs.
- Most infections in endemic areas are subclinical.
Important Facts
- The geographic distribution of the fungus includes Southwestern U.S., Northern Mexico, and Central and South America.
- The fungus likes to live in these regions because the soil is arid to semiarid, sandy and alkaline, the environmental temperature is high, with low rainfall, and low elevations above the sea level.
- Animals inhale the fungus arthrospores from the soil – in the body temperature the arthrospores are transformed into spherules that mature to form hundreds of endospores – the spherule wall eventually ruptures and the endospores attract neutrophils and macrophages to the site – if the animals do not mount an effective immune response, the endospores disseminate via the lymphatic and blood vessels causing systemic disease.
- Most infections in endemic areas are subclinical.
-
Animal Species Affected
- Coccidioidomycosis can occur in dogs (most prevalent), cats, horses and other animal species.
-
Clinical Signs
- Dog:
- There is no age, sex or breed predilection but young adult dogs of large breeds appear more frequently in case series possibly because they are more exposed to the fungus ecological niche.
- Most dogs in endemic areas have sub-clinical disease or sub-acute to chronic mild disease.
- Non-specific signs include fever, anorexia, weight loss, depression. These signs can be mild in dogs living in endemic areas and may be present intermittently for years before veterinary assistance is sought.
- Respiratory signs are common and include dry or productive coughing, tachypnea, increased lung sounds, exercise intolerance, and increased respiratory efforts.
- Disseminated disease is uncommon in dogs. Common sites of dissemination include bone/joints, peripheral lymph nodes, eyes, skin, pericardium, testes, prostate, and central nervous system. A history of respiratory signs may be absent in dogs with disseminated disease.
- Dog:

-
-
- Skin lesions are rare and include nodules, cold abscesses, draining tracts and ulcers. Skin lesions are often present over sites of bone involvement.
-

-
-
- Infection can be confined to the respiratory tract and can spontaneously resolve.
-
-
- Cat:
- Coccidioidomycosis is less common in cats than in dogs.
- There is no age, sex or breed predilection.
- Most reported cases have been FIV and FeLV negative.
- Skin lesions are common (~50%) in cats and they are not often associated with adjacent bone involvement. Lesions reported include subcutaneous nodules, abscesses, and draining lesions.
- Other reported signs include fever (~31%), increased respiratory effort or tachypnea (25%), lameness (<20%), and ocular abnormalities (13%).
- Few cats were reported with neurologic signs.
- Dissemination to abdominal organs can occur.
- Many cats have disseminated disease at the time of diagnosis.
- Cat:
Important Facts
- Most dogs in endemic areas have sub-clinical disease or sub-acute to chronic mild disease.
- Respiratory disease is very common in dogs but dissemination to other organs is uncommon.
- Coccidioidomycosis is uncommon in cats and many cats have disseminated disease at the time of diagnosis.
-
Diagnosis
- Radiographs:
- Thoracic radiograph shows an interstitial or miliary to nodular pattern.
- Hilar lymphadenomegaly is common.
- Radiographs:
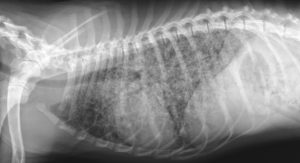
-
-
- Radiograph of the extremities shows a productive/lytic lesion.
-

-
- Cytology and histopathology: finding organisms in various samples is the gold standard test; however, the sensitivity is low.
- Presence of pyogranulomatous inflammation and spherules with endospores in cytology or histopathology is diagnostic. However, fungal elements are rarely found in cytological exams but are usually present histologically but may be sparse. Aspirates from enlarged lymph nodes or impression smears from draining skin lesions have a better chance of a positive yield.
- Special stains:
- Cytology: Papanicolaou, Wright or Periodic Acid Shiff (PAS) stains.
- Histopathology: H&E, PAS or Gomori methenamine silver (GMS) stains. To learn about the characteristic of the yeast in histology refer to the review article by Hoffmann et al, 2023.
- Special stains:
- Presence of pyogranulomatous inflammation and spherules with endospores in cytology or histopathology is diagnostic. However, fungal elements are rarely found in cytological exams but are usually present histologically but may be sparse. Aspirates from enlarged lymph nodes or impression smears from draining skin lesions have a better chance of a positive yield.
- Cytology and histopathology: finding organisms in various samples is the gold standard test; however, the sensitivity is low.
-
- Serologic antibody tests:
- Antigens used:
- Tube precipitin (measure IgM). Becomes positive within 2 weeks and negative 4-5 weeks post-infection.
- Protein complement fixation (measure IgG). Becomes positive after 8-12 weeks.
- Tests used:
- Agar gel immunodiffusion (AGID) test for IgM and IgG antibodies – best one for dogs. Sensitivity of 90-95%.
- Complement fixation test – Many false positives in dogs. Good for cats.
- Antibody titers usually range from 1:2 to 1:256. There is no correlation in dogs between disease severity and antibody titers. However, a titer > 1:16 is highly suggestive of clinically relevant coccidioidomycosis in ill dogs.
- An enzyme immunoassay (EIA – MiraVista Labs, Indianapolis Indiana) antibody test to detect canine IgG reacting to Coccidioides antigens has shown a sensitivity of 89.2% and specificity of 97.2%. This test is faster than the AGID test.
- A point-of-care serologic antibody test (sona Coccidioides antibody lateral flow assay [IMMY, Norman, Oklahama) was developed and showed good agreement with the standard AGID test for positive cases (88.9%) and negative cases (100%). Dogs with low AGID titers are more likely to be negative on the point-of-care test, which will require additional tests to confirm the presumptive clinical diagnosis.
- Antigens used:
- Culture – attempts should not be made to culture the organism in veterinary practices because of the risk for human infection. Fungal culture is rarely needed but if deemed necessary submit the sample(s) to a laboratory with the patient’s detailed history and clinical signs.
- Serologic antibody tests:
Important Facts
- The patient’s detailed history and clinical signs are important diagnostic tools.
- Cytology of aspirates or direct smears of exudate and histology reveal a pyogranulomatous inflammation with or without fungal elements.
- The sensitivity of finding the organism on cytology and histopathology is low.
- Radiographic findings are not pathognomonic but can support a presumptive diagnosis.
- Agar gel immunodiffusion test for IgM and IgG antibodies has good sensitivity.
- Culture is rarely needed.
-
Treatment
- Fluconazole: best choice for cases with central nervous system or ocular involvement
- Dogs: 5 – 10 mg/kg q 12h.
- Cats: 10 mg/kg q 12h or 50 mg q 24 h (cat < 4 kg); 100 mg q 24h (cat > 4 kg)
- Itraconazole:
- Dogs and cats: 5 mg/kg q 12-24 h.
- Excellent choice in cats and for cases with bone involvement.
- Oral formulation with cyclodextrin carrier has better bioavailability.
- Amphotericin B:
- Dose: deoxycholate formulation:
- Dogs: 0.5 mg/kg IV q 48h
- Cumulative dose: 5-10 mg/kg
- Cats: 0.25 mg/kg IV q 48h
- Cumulative dose: 4-8 mg/kg.
- Dogs: 0.5 mg/kg IV q 48h
- Good option in cases of severe disease or azoles do not work as sole therapy.
- Dose: deoxycholate formulation:
- Posaconazole or Voriconazole:
- Posaconazole is a newer triazole structurally related to itraconazole.
- Dose:
- Dogs: 5-10 mg/kg q 12-24h.
- Cats: 5 mg/kg q 24h.
- Side effects:
- Inappetence, vomiting, diarrhea and increase in liver enzymes.
- Monitor liver enzymes during treatment.
- Voriconazole is a newer triazole structurally related to fluconazole.
- Dose:
- Dogs: 4-5 mg/kg q 12h. Cats: 2.68 to 5.10 mg/kg q 72-96h or 12.5 mg/cat q 72h. The dose for unusually large or small cats should be based in mg/kg and not mg/cat. At this dose regimen of q 72-96h, the reported side effects are fewer and less severe and include hyporexia, weight loss, and less commonly ALT increase.
- Cats treated with voriconazole at the dose range of 4.32 mg/kg to 13 mg/kg q 24h are prone to develop various side effects that include one or more of the following: inappetence, mydriasis, apparent blindness, ataxia, nystagmus, tremors, pelvic limb paralysis, cutaneous drug reaction, azotemia, decreased menace and decreased pupillary reflexes.
- Monitor liver enzymes during treatment.
- Terbinafine
- It has shown to have a synergistic effect with azoles.
- Consider using as a salvage drug to increase the effect of azoles.
- Dose: It can be given with or without food
- Dogs: 35-50 mg/kg q 24h.
- Cats: half of 500 mg tablet (i.e. 250 mg q 24h).
- Treat at least 30 days past clinical resolution of signs. Resolution of clinical signs and titer ≤ 1:2 indicate cure.
- Treatment may be unnecessary for animals with lesions confined to the respiratory tract because spontaneous resolution is common.
- Fluconazole: best choice for cases with central nervous system or ocular involvement
Important Facts
- Azoles generally work well for the treatment of coccidioidomycosis.
- Fluconazole should be considered in cases of ocular or central nervous system involvement.
- Amphotericin B can be used in severe cases or cases that do not respond solely to azoles.
- Terbinafine has shown to have a synergistic effect with azoles and should be considered as a salvage drug to increase the efficacy of azoles.
- Treat for at least 30 days post clinical resolution of signs.
- Resolution of clinical signs and titer ≤ 1:2 indicate cure.
-
Prognosis
- Generally good with treatment.
- Recovery rate is about 60%.
- Prognosis is guarded to poor if central nervous system is affected.
References
Arbona N, Butkiewicz CD, Keyes M et al. Clinical features of cats diagnosed with coccidioidomycosis in Arizona, 2004-2018. J Fel Med Surg 2019; https://doi.org/10.1177/1098612X19829910
Barrs VR, Bęczkowski PM, Talbot JT et al. Invasive fungal infections and oomycoses in cats. 1. Diagnostic approach. J Fel Med Surg 2024; doI: 10.1177/1098612X231219696
Barrs VR, Hobi S, Wong A et al. Invasive fungal infections and oomycoses in cats. 2. Antifungal therapy. J Fel Med Surg 2024; doI: 10.1177/1098612X231220047
Easterwood LF, Harkin KR, Rankin AJ. Oral voriconazole therapy in cats with histoplasmosis yielded mild side effects and a favorable outcome. J Am Vet Med Assoc 2023; doi.org/10.2460/javma.23.05.0276.
Greene CE. Infectious Diseases of the Dog and Cat. 4th ed. St. Louis, Missouri, Elsevier, Saunders, 2012.
Greene RT, Troy GC. Coccidioidomycosis in 48 cats: a retrospective study (1984-1993). J Vet Intern Med 1995; 9: 86-91.
Hoffmann AR, Ramos MG, Walker RT et al. Hyphae, pseudohyphae, yeasts, spherules, spores, and more: A review on the morphology and pathology of fungal and oomycete infections in the skin of domestic animals. Vet Pathol 2023; doi.org/10.1177/03009858231173715
Holbrook ED, Greene RT, Rubin SI, et al. Novel canine anti-Coccidioides immunoglobulin G enzyme immunoassay aids in diagnosis of coccidioidomycosis in dogs. Med Mycol 2019; 57: 800-806. doi: 10.1093/mmy/myy157
Kirsch EJ, Greene RT, Prahl A, et al. Evaluation of Coccidioides antigen detection in dogs with coccidioidomycosis. Clin Vaccine Immunol 2012; 19: 343–345.
Miller WH, Griffin CE, Campbell KL. Muller & Kirk’s Small Animal Dermatology. 7th ed. St. Louis, Missouri, Elsevier, Mosby, 2013.
Reagan K, McHardy I, Thompson III GR et al. Clinical performance of a point-of-care Coccidioides antibody test in dogs. J Vet Intern Med 2021; DOI: 10.1111/jvim.16087
Rippon JW. Medical Mycology. Philadelphia, WB Saunders, 1988.
Scott DW. Large Animal Dermatology. Philadelphia, WB Saunders, 1988.
Shubitz LF, Schlacks S, Vishkautsan P, et al. Posaconazole treatment of refractory coccidioidomycosis in dogs. J Vet Intern Med 2021; DOI: 10.1111/jvim.16282
Shubitz LF, Schlacks S, Vishkautsan P, et al. Erratum for “Posaconazole treatment of refractory coccidioidomycosis in dogs”. J Vet Intern Med 2022; DOI: 10.1111/jvim.16393
Vishkautsan P, Papich MG, Thompson GR III et al. Pharmacokinetics of voriconazole after intravenous and oral administration to healthy cats. Am J Vet Res 2016; 77: 931–939.

