4.4 Systemic Mycosis – Blastomycosis – Small Animals
Learning Objectives
- Know the endemic areas for blastomycosis in the US.
- Know that blastomycosis is caused by Blastomyces dermatitidis, which is a thick-walled, broad based budding yeast of about 5 to 20 µm in diameter.
- Learn the disease pathogenesis.
- Remember that primary cutaneous inoculation is rare. However, you may see cases in which only the skin is affected. Lesions will be usually present at the paws and legs. Chronic cases may be associated with involvement of the adjacent bone.
- Be able to recognize the disease clinically.
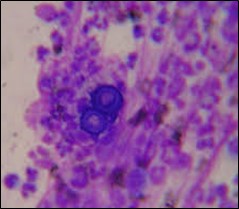
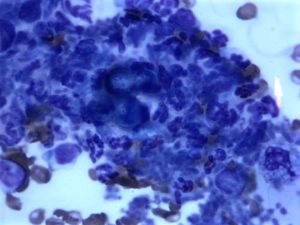
- Remember! Cytology of aspirates of lymph node or lung and impression of skin exudate usually reveals the thick-walled, broad-based budding yeast. Biopsy can be performed if the cytological exam failed to demonstrate the organism. Neutrophils and macrophages are seen with the yeast.
- Know how to manage this condition.
- Remember! Blastomycosis is a severe disease. Animals can die from it. It is important that you learn about the prognosis of this disease in order to be able to discuss that with your client.
-
General Considerations
- Blastomycosis is a systemic fungal disease of primarily North America. However, it has been identified in Africa and Central America.
- The reservoir is thought to be moist, sandy and acid soils. Decaying vegetation and animal waste help the fungus growth.
Important Facts
- Blastomycosis is a systemic fungal infection of primarily North America.
- Blastomyces dermatitidis lives in moist, sandy and acid soils.
-
Etiology and Pathogenesis
- Blastomycosis is caused by Blastomyces dermatitidis.
- The organism is a dimorphic saprophytic fungus:
- At body temperature, it is a broad based budding yeast measuring 5 to 20 µm in diameter. Its cell wall is thick, refractile, and has a double-contour.
-
-
- In the soil, it is a mycelium.
-
-
- The main mode of infection is through inhalation of the fungus from the soil. Once in the lungs, Blastomyces dermatitidis disseminates via lymphatic and blood vessels to various organ systems.
- Primary cutaneous inoculation may occur in humans, dogs and cats from bite wounds, other kinds of skin trauma or during necropsies.
Important Facts
- The main route of infection is inhalation of the fungus mycelium present in the soil.
- Primary cutaneous inoculation is rare.
-
Geographic Distribution
- Ohio, Missouri, Mississippi, and St. Lawrence river valleys.
- Middle atlantic states.
- Canadian provinces of Quebec, Manitoba, and Ontario.
-
Epidemiology
- Proximity to water is an important risk factor. In a Wisconsin study, 95% of dogs with blastomycosis lived about 400m of a water source. In another study, dogs with blastomycosis were 10 times more likely to live within 400m of water.
- Excavation also increases the risk for infection.
- Strictly indoor dogs and cats can develop blastomycosis by playing with contaminated pot soil, for example.
- The fungus does not seem to be widely distributed in endemic areas.
- Most people and dogs living in endemic areas show no evidence of exposure determined by serologic or skin test.
-
Species Affected
- Humans, dogs, cats and horses. Dogs are more susceptible than humans and cats likely because they often keep their nose close to the ground, which increases their chances to inhale a larger inoculum.
-
Signalment and Clinical Signs
- Dog:
- Young male dogs of large and sporting breeds are predisposed.
- Primary pulmonary disease is typically asymptomatic.
- Disseminated disease presents as follows:
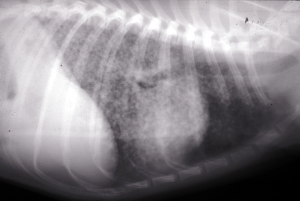
- Respiratory signs are common and characterized by coughing and dyspnea. Lung lesions are typically characterized by a diffuse miliary to nodular interstitial pattern.
- Dog:
-
-
-
- Fever and hyporexia or anorexia are commonly present. Weight loss will develop in chronic cases.
- Lymphadenomegaly of one or more lymph nodes is a common finding.
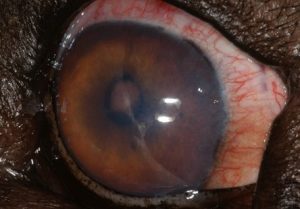
- Ocular lesions occur in about 40% of the cases and are characterized by uveitis, retinal detachment and retinal granulomas.
-
-

-
-
-
- Lameness due to bone involvement has been reported in about 30% of the cases.
- Skin disease occurs in about 50% of the dogs. Nodules and plaques that may ulcerate are common. Lesions mimicking deep pyoderma with draining sinus tracts may develop. Subcutaneous abscesses can also be seen. Skin lesions can be found anywhere but the nasal planum, face, and nail folds appear to be preferred sites.
-
-




-
-
- Primary cutaneous inoculation is rare. Usually the extremities are affected. Lesions will be limited to the skin but chronic cases may also have bone changes.
-

-
-
- Tissues less often infected include testes, prostate, kidneys, urinary bladder, brain and nasal passages.
- Lesions have been found in most organs of infected animals with the exception of the stomach and intestinal tract.
-
Important Facts
- Clinical signs are non-specific and usually include hyporexia or anorexia, weight loss, fever, coughing, dyspnea, ocular disease, lameness, and skin disease.
- Skin disease occurs in about 50% of the cases and includes nodules, plaques with ulceration and draining tracts.
- Lymphadenomegaly of one or more lymph nodes is a common finding.
- Primary cutaneous inoculation is rare and lesions are usually present on the extremities.
-
-
Cats:
- Cats appear to be more resistant to infection than dogs.
- There is no age, breed or sex predilection.
- Respiratory signs are common and some cases show neurologic and ocular signs.
- Skin lesions have also been reported and are characterized by nodules and/or plaques that can ulcerate and drain.
- The disease is usually advanced at the time of diagnosis.
-


Important Facts
- Cats appear to be more resistant to infection than dogs.
- They usually present with respiratory signs and the disease is generally advanced at presentation.
-
Diagnosis
- Signalment, history and clinical signs.
- Thoracic radiographs: typically shows miliary to interstitial pattern.
- Aspirate cytology of lymph nodes, skin nodules and plaques, lungs or impression smear of cutaneous draining lesions. Findings include double-walled, broad based, budding yeasts associated with a pyogranulomatous inflammation. Blastomyces dermatitidis organisms are found in more than 50% of the time.
-
- Organisms can also be identified in airway wash. They can also be found in urine samples in the presence of prostatic, bladder, or renal involvement.
- Biopsy of skin lesions and/or lymph nodes show pyogranulomatous inflammation surrounding thick-walled, broad based and budding yeasts. To learn about the characteristic of the yeast in histology refer to the review article by Hoffmann et al, 2023.
- Culture of cytological specimens is not recommended for in-clinic laboratories because of the danger of infection from the mycelial form of the organism. However, samples can be sent to a laboratory for culture. Clearly state in the request that you are suspecting of blastomycosis.
- Other tests:
- Only after an extensive search for the organism has been made should urine or serologic antigen and antibody testing be performed.
- A commercial ELISA immunoassay test (EIA, MiraVista Diagnostics, Indianapolis, Indiana) that detects Blastomyces antigen in the urine and serum has generally replaced the agar-gel immunodiffusion (AGID) test in the diagnosis of canine blastomycosis. In a study, the sensitivity of the urine test was 93.7% and of the serum 87.0%. The antigen urine test is the preferred sample due to better sensitivity but serum can also be used. The specificity of the EIA test is only about 75% due to cross reactivity with Histoplasma spp organisms. However, the specificity is 95% to 100% in healthy dogs and dogs with nonfungal pulmonary disease.
- AGID test detects antibodies against Blastomyces dermatitidis organisms. The sensitivity of this test can be as low as 17.4% in the dog.
Important Facts
- The characteristic history and clinical signs are usually confirmed by cytology of aspirates (lymph node, skin, lung), impression smear of cutaneous exudate or by biopsies of skin and/or lymph nodes.
- Cytology and histopathology will show a pyogranulomatous inflammatory infiltrate associated with thick-walled, broad-based, budding yeast.
- Fungal culture may be needed to confirm a presumptive diagnosis.
- Serum or urine Blastomyces antigen test has good sensitivity (especially the urine test) and should be used when organisms cannot be found after extensive search through various test.
-
Treatment
- Itraconazole (do not use compounded formulations) :
- Efficacy: It is as good as amphotericin B but better than ketoconazole and fluconazole.
- Dose: Dogs: 5 mg/kg orally q 12h for 5 days, then q 24h. Cats: 5 mg/kg q 12-24h. Give the capsule formulation with food.
- Treat for at least 30 days after all signs of disease have resolved. Most dogs are treated for 2 to 3 months.
- Recurrence rate is about 20-25% within the first year.
- Side effects:
- Most common side effects are anorexia and hepatotoxicity.
- Cutaneous vasculitis can occur in about 7.5% of dogs receiving 10 mg/kg q 24h or higher doses. The lesions can mimic the cutaneous lesions associated with blastomycosis.
- Monitor liver enzymes during treatment.
- Itraconazole (do not use compounded formulations) :

-
- Amphotericin B:
- Efficacy: similar to itraconazole.
- It should be used in severe, disseminated disease especially when the central nervous system is affected. It is an option in cases that do not respond or tolerate azole therapy.
- Dose (Deoxycholate):
- Dogs: 0.5 mg/kg every other day. Cats: 0.25 mg/kg every-other-day.
- Cumulative dose – 8 to 10 mg/kg.
- Dose (Lipid-complex injection):
- Dogs: 2-3 mg/kg IV 3 days per week for a total of 9-12 treatments (cumulative dosage of 24-27 mg/kg).
- Cats: 1 mg/kg IV 3 days per week for a total of 12 treatments (cumulative dosage of 12 mg/kg).
- Dosage used can be higher because of the lower nephrotoxicity of the lipid-based formulation.
- Amphotericin B is preferred over itraconazole in cases with severe respiratory or neurologic signs, that are vomiting or that failed to respond to itraconazole.
- Recurrence rate is similar to itraconazole (20-25% within the first year).
- Side effects:
- Nephrotoxic (less frequent with the lipid-based formulation).
- Acute infusion related adverse events: fever, vomiting, myalgia, muscle tremors, phlebitis, and anaphylaxis.
- Side effects can be minimized by using the lipid-complexed formulations (Abelcet®).
- Discontinue treatment if BUN is greater than 50 mg/dl.
- Fluconazole:
- Efficacy was similar to itraconazole in one study but time to disease resolution was longer.
- Dose:
- Dogs: 5-10 mg/kg q 12h. Cats: 50 mg/cat q 12-24h.
- A retrospective study compared the efficacy and cost of treating dogs with blastomycosis with itraconazole and fluconazole, both drugs at dose range of 5 to 10 mg/kg/day. More dogs taking fluconazole (25%) compared to itraconazole (10%) died during the first 2 weeks of treatment. Ninety percent of the dogs treated with itraconazole and 75% of the dogs treated with fluconazole achieved remission and this difference was not statistically significant. Treatment duration was significantly longer for fluconazole (183 days) compared to itraconazole (138 days). Hepatotoxicity (increase in ALT) was similar for both treatments. Costs for fluconazole (generic) were significantly lower than for itraconazole (brand name – generic drug is associated with unpredictable absorption). Fluconazole can be an option for blastomycosis cases where owners have important monetary concerns. In addition, it has better penetration into the cerebral nervous system and ocular tissues.
- Side effects:
- Generally well tolerated. Vomiting, diarrhea and increase in liver enzymes.
- Monitor liver enzymes during treatment.
- Posaconazole or voriconazole
- Posaconazole is a newer triazole structurally related to itraconazole.
- Dose:
- Dogs: 5-10 mg/kg q 12-24h. Cats: 5 mg/kg q 24h.
- Side effects:
- Inappetence, vomiting, diarrhea and increase in liver enzymes.
- Monitor liver enzymes during treatment.
- Voriconazole is a newer triazole structurally related to fluconazole.
- Dose:
- Dogs: 4-5 mg/kg q 12h. Cats: 2.68 to 5.10 mg/kg q 72-96h or 12.5 mg/cat q 72h. The dose for unusually large or small cats should be based in mg/kg and not mg/cat.
- Cats treated with voriconazole at the dose range of 4.32 mg/kg to 13 mg/kg q 24h are prone to develop various side effects that include one or more of the following: inappetence, mydriasis, apparent blindness, ataxia, nystagmus, tremors, pelvic limb paralysis, cutaneous drug reaction, azotemia, decreased menace and decreased pupillary reflexes.
- Monitor liver enzymes during treatment.
- Terbinafine
- It has shown to have a synergistic effect with azoles.
- Consider using as a salvage drug to increase the effect of azoles.
- Dose: It can be given with or without food
- Dogs: 35-50 mg/kg q 24h
- Cats: half of 500 mg tablet (i.e 250 mg q 24h).
- Duration of therapy
- Treat all cases for at least 30 days past resolution of clinical signs, resolution of imaging abnormalities, and 2 or 3 negative Blastomyces urine or serum antigen test (EIA). It is also recommended that animals should be treated for at least 6 months.
- Recurrence of the disease usually occurs within six months to one year of completion of therapy.
- The commercial ELISA immunoassay test (EIA, MiraVista Diagnostics) that detects Blastomyces antigen in the urine can also be used to monitor response to therapy and relapse.
- Amphotericin B:
Important Facts
- Itraconazole alone is efficacious but fluconazole, amphotericin B and/or ketoconazole can also be treatment options.
- Posaconazole or voriconazole can be used in cases refractory to other treatments.
- Use voriconazole carefully in cats due to potential severe side effects.
- Treat these cases for at least 30 days past clinical resolution of clinical signs and 2 or 3 negative Blastomyces urine or serum antigen test.
-
Prognosis
- About 20% to 30% of the cases may relapse within one year of completion of therapy. Most cases relapse within the first 6 months.
- Severity of lung disease correlates with relapse. About 50% of the patients die of respiratory failure during the first 7 days of therapy.
- If ocular disease is present the risk for relapse increases.
- The prognosis is good if the animal survives the first week of therapy.
- Poor if the central nervous and cardiac systems are involved and lung disease is severe.
Important Facts
- 20% to 30% of the cases may relapse within 6 months to 1 year after completing therapy.
- Prognosis is worse if the central nervous and cardiac systems are affected and if the lung lesions are severe.
- The presence of ocular disease increases the chances for relapse.
- Prognosis is generally good if the animal survives the first week of therapy.
References
Barrs VR, Bęczkowski PM, Talbot JT et al. Invasive fungal infections and oomycoses in cats. 1. Diagnostic approach. J Fel Med Surg 2024; doI: 10.1177/1098612X231219696
Barrs VR, Hobi S, Wong A et al. Invasive fungal infections and oomycoses in cats. 2. Antifungal therapy. J Fel Med Surg 2024; doI: 10.1177/1098612X231220047
Easterwood LF, Harkin KR, Rankin AJ. Oral voriconazole therapy in cats with histoplasmosis yielded mild side effects and a favorable outcome. J Am Vet Med Assoc 2023; doi.org/10.2460/javma.23.05.0276.
Foy DS, Trepanier LA, Kirsch EJ et al. Serum and urine Blastomyces antigen concentrations as markers of clinical remission in dogs treated for systemic blastomycosis. J Ver Intern Med. 2014; 28:305-310.
Greene CE. Infectious Diseases of the Dog and Cat. 4th ed. St. Louis, Missouri, Elsevier, Saunders, 2012.
Hoffmann AR, Ramos MG, Walker RT et al. Hyphae, pseudohyphae, yeasts, spherules, spores, and more: A review on the morphology and pathology of fungal and oomycete infections in the skin of domestic animals. Vet Pathol 2023; doi.org/10.1177/03009858231173715
Langlois DK, Pelosi A, Kruger JM et al. Successful treatment of intracardiac and intraocular blastomycosis in a dog with combination azole therapy. J Am Anim Hosp Assoc 2013; 49: 273–280.
Mazepa A.S.W. et al. Retrospective comparison of the efficacy of fluconazole or itraconazole for the treatment of systemic blastomycosis in dogs. J. Vet. Intern. Med. 25:440-45, 2011.
Motschenbacher LO, Furrow E, Rendahl AK et al. Retrospective analysis of the effects of Blastomyces antigen concentration in urine and radiographic findings on survival in dogs with blastomycosis. J Vet Inernt Med. 2021. DOI: 10.1111/jvim.16041
Rippon JW. Medical Mycology. Philadelphia, WB Saunders, 1988.
Miller WH, Griffin CE, Campbell KL. Muller & Kirk’s Small Animal Dermatology. 7th ed. St. Louis, Missouri, Elsevier, Mosby, 2013.
Scott DW. Large Animal Dermatology. Philadelphia, WB Saunders, 1988.
Vishkautsan P, Papich MG, Thompson GR III et al. Pharmacokinetics of voriconazole after intravenous and oral administration to healthy cats. Am J Vet Res 2016; 77: 931–939.

