4.8 Cutaneous and Subcutaneous Mycosis – Sporotrichosis – Small Animals
Learning Objectives
- Know that fungi of the Sporothrix schenckii species complex are a soil and plant saprophyte that gain entrance in the host by wound contamination through various sources. However, infection can also occur via inhalation of fungal spores.
- Remember! Sporotrichosis is a zoonosis. Cats can transmit the disease more easily to people than dogs because large numbers of organisms are present in exudate from cat’s skin lesion exudate.
- Know that the cutaneous and cutaneous-lymphatic forms of the disease occur more frequently but in endemic areas the systemic form is common, especially in cats. Describe the three forms of the disease.
- Remember! The small pleomorphic yeasts are rarely found on cytological exam from impression smears or skin biopsies with the exception of cats. Preferred stains for demonstration of the organism are periodic acid Schiff (PAS) or Gomori methenamine silver (GMS). Know that fungal culture is an accurate diagnostic test and it identifies the fungal species, which is important for epidemiologic reasons.
- Learn how to manage sporotrichosis.
-
Etiology and Pathogenesis
- Sporotrichosis is caused by organisms of the Sporothrix (S) species that belong to the clinical and environmental clades. The clinical clade includes S. brasiliensis, S. schenckii, S. globosa, and S. luriei, which frequently cause infection in humans and animals. The environmental clade rarely causes infection in mammals and includes S. chilensis, S. mexicana, S. humicola, and S. pallida. Species vary in virulence and distribution. The organism is pleomorphic and the cigar shape is the characteristic form.
-
- The fungus lives as a soil and plant saprophyte.
- It is dimorphic (i.e. yeast at 37°C and mycelium at 25°C).
- Infection occurs primarily via traumatic inoculation into body tissues of contaminated soil, plant material, nails, organic matter and bites of sick animals (especially cat to cat and cat to human transmission). Inhalation can also be a mode of infection.
- Animal to people transmission is possible, especially from cats because large numbers of organisms are present in the exudate from cat lesions!


Important Facts
- Organisms of the Sporothrix schenckii species complex are the causative agents.
- The fungus is a soil and plant saprophyte and infection occurs primarily via wound contamination.
- Sporotrichosis is a zoonosis and cats can transmit the disease more easily to people than dogs because large numbers of organisms are present in exudate from cat lesions.
-
Natural reservoir
- Sporothrix organisms prefer moist soil rich in decaying plant material.
- They have been isolated from rose bush thorns, sphagnum moss, tree bark, and mine timbers.
-
Geographic distribution
- Tropical and temperate zones around the world, especially in the Americas. It is uncommon in Europe.
-
Animal Species Affected
- The disease has been reported in cats (very susceptible), dogs, horses, humans and a variety of mammalian and avian species.
-
Clinical Signs
- Three clinical forms:
- Cutaneous ans subcutaneous:
- The infection is limited to the skin and subcutaneous tissues and lesions can be localized or generalized.
- Most cats will develop multiple nodules, ulcers, and crusts as a result of autoinoculation during grooming.
- In cats, extensive areas of skin necrosis can occur, exposing muscle and bone.
- Cutaneous ans subcutaneous:
- Three clinical forms:


-
-
- Cutaneous-lymphatic:
- Firm round nodules at the point of entry.
- Nodules progress to the subcutaneous tissues and lymphatics.
- Usually associated with regional lymphadenomegaly.
- Cutaneous-lymphatic:
-


-
- Systemic:
- It is rare and most frequently seen in cats.
- Bone, lung, liver, spleen, kidneys, testes, mucosal sites, gastrointestinal tract, central nervous system and skin can be affected. Skin lesions will be typically multifocal because of systemic dissemination of fungal organisms via blood and lymphatic vessels.
- Systemic:
Important Facts
- Cats are very susceptible to sporotrichosis.
- Three clinical forms including cutaneous, cutaneous–lymphatic and systemic disease.
- Most cutaneous lesions are characterized by nodules that eventually ulcerate and drain.
- Areas of skin necrosis can occur exposing muscle and bone.
- The systemic form is seem more often in cats.
-
Diagnosis: Antifungal treatments may decrease the sensitivity of the diagnostic tests discussed below
- Cytology:
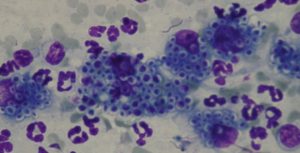
- The organisms are difficult to detect in samples from dogs but easy in samples from cats (80%) because they are in large numbers.
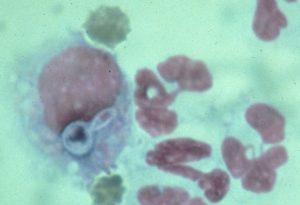
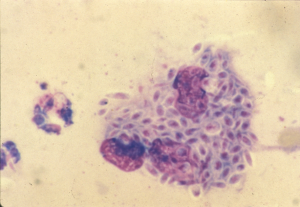
- Pyogranulomatous inflammation is present. The fungal organisms are pleomorphic (i.e. oval, round, cigar-shaped) small yeast 3-5 µm wide and 5-10 µm long. They can be found inside macrophages or extracellularly.
- Cytology:
-
- Skin Biopsy:
- It is difficult to find the organisms in the skin tissue of dogs (< 20%), but it can be present in > 60% of cats’ skin tissue. Sample early lesions to increase the chances to find the organisms. Special stains such as periodic acid Schiff or Grocott methenamine silver stains should be request if yeasts cannot be visualized in H&E stain. To learn about the characteristic of the yeast in histology refer to the review article by Hoffmann et al, 2023
- A pyogranulomatous inflammation with pleomorphic yeast present inside macrophages or extracellularly is diagnostic.
- Culture:
- The reference standard method is the mycological test, which is based on the Sporothrix spp. isolation in culture media, its identification by morphological parameters and the culture conversion to the yeast phase.
- The yeast grows readily in Sabouraud’s dextrose agar at 25°C to 30°C.
- Samples submitted for culture should include both a sample of the exudate (from deep within a draining tract) and a piece of tissue (removed surgically) for a macerated tissue culture.
- Sporothrix sp. is a slow growing organism and because the conversion to the yeast phase is required, the definitive diagnosis may take as long as 30 days.
- Immunohistochemistry and PCR should be used if the characteristic yeast organisms cannot be found on cytology and histopathology. However, these tests may not be provided by all laboratories. Tissues for PCR should be frozen at minus 20ºC. The PCR test will allow for species identification of Sporothrix.
- A serological test for the preliminary diagnosis of feline sporotrichosis has been validated for all clinical forms of sporotrichosis. This ELISA test detects antibodies against a purified antigen of Sporothrix spp.
- More than one diagnostic test may be needed before a diagnosis can be confirmed.
- Differential diagnosis:
- Other mycoses.
- Neoplasia.
- Mycobacteriosis.
- Skin Biopsy:
Important Facts
- Cytology of exudate and histopathology are sensitivity tests in cats since they generally carry large numbers of organisms in exudate and skin samples but the sensitivity of these tests is low for other species.
- Culture from tissue and exudate samples is the reference diagnostic test but results may take as long as 30 days.
- Immunohistochemistry and PCR can be used if cytology and histopathology are negative. However, they are not widely available at this time.
- Diagnosis can also be made by a validated serological ELISA test for the preliminary diagnosis of feline sporotrichosis.
-
Treatment
- Itraconazole:
- Mainstay drug for cats and dogs and its efficacy as monotherapy has been demonstrated.
- Cats and dogs: 5 mg/kg q 12-24 h
- Do not use compounded formulations because they are not effective.
- Give it with food if using capsules. The liquid formulation with cyclodextrin carrier has better bioavailability.
- It can be used with potassium iodide in more severe cases.
- Combination therapy with itraconazole and cryosurgery has been effective.
- Monitor liver enzymes during treatment.
- Potassium iodide:
- Dog: potassium iodide (supersaturated oral solution): 40 mg/kg q 12h or q 8h.
- Cat: potassium iodide (supersaturated oral solution): 10-20 mg/kg q 12h.
- If combined with itraconazole and using the capsule formulation:
- Dogs and cats: 2.5 – 20 mg/kg q 24h (start with 2.5 mg/kg q 24h and gradually increase the dose every 30 days by 2.5 mg/kg q 24h until clinical response is achieved or until the dose reaches 20 mg/kg q 24h)
- Cats are more susceptible to iodism. Signs of iodism include vomiting, anorexia, ptyalism, depression, twitching, hypothermia, dry hair coat with excess scaling of the skin, and cardiovascular failure.
- Fluconazole:
- Dogs: 5 – 10 mg/kg q 12h.
- Cats: 10 mg/kg q 12h or 50 mg q 24 h (cat < 4 kg); 100 mg q 24h (cat > 4 kg).
- Monitor liver enzymes during treatment.
- Amphotericin B:
- Dose: deoxycholate formulation:
- Dogs: 0.5 mg/kg IV q 48h
- Cumulative dose: 5-10 mg/kg
- Cats: 0.25 mg/kg IV q 48h
- Cumulative dose: 4-8 mg/kg.
- Dogs: 0.5 mg/kg IV q 48h
- Dose: deoxycholate formulation:
- Terbinafine
- It has shown to have a synergistic effect with azoles.
- Consider using as a salvage drug to increase the effect of azoles.
- Dose: It can be given with or without food
- Dogs: 35-50 mg/kg q 24h
- Cats: half of 500 mg tablet (i.e 250 mg/day)
- Ketoconazole:
- Dose:
- Dogs: 10 to 15 mg/kg q 12h
- Cats: 5-10 mg/kg q 12h
- Use in dogs that cannot tolerate or fail to respond to iodides
- Cats have more side effects with ketoconazole; try to avoid it.
- Monitor liver enzymes during treatment.
- Dose:
- Treat for 4 to 8 weeks after resolution of all clinical signs. Reported mean treatment duration is 4 months. Some cases may require > 1 year of therapy.
- Cats clinically cured should be neutered/spayed to reduce the instinct for hunting, fighting, mating, roaming and thus acquiring or transmitting the disease.
- Itraconazole:
-
Prognosis
- > 70% of cats and 80% of dogs can be cured of the disease if an adequate treatment regimen is instituted.
- In general, lesions localized to the nasal region of cats are difficult to treat. The severity and extension of the lesions, high fungal loads, and extension of lesions to mucosa, cartilage, and bone may impede their healing.
- Presence of respiratory signs have been associated with a twofold increase in death rate.
- Relapse or re-infection can occur 3 to 18 months after therapy discontinuation.
-
Public Health Considerations
- Sporotrichosis is a zoonosis.
- Cats are at higher risk to transmit the disease to people because copious numbers of organisms are found in exudate and tissues from many cats.
- Population at greatest risk include veterinarians, their assistants, and anyone exposed during treatment.
- Appropriate physical restraint or sedation of patients that do not cooperate must be done to allow a thorough physical examination and proper sample collection.
- Wear disposable gloves when handling cats with draining lesions and wash with soap arms and hands after handling cats with draining lesions.
- Cages and transport containers must be decontaminated for at least 10 minutes with 1% sodium hypochlorite diluted 1:3 in water.
- Surfaces where the affected animal had contacted need to be disinfected with 1% sodium hypochlorite solution followed by 70% alcohol for at least 10 minutes using disposable paper towels.
Important Facts
- Itraconazole is the mainstay treatment for cats and dogs.
- Potassium iodide can be used as monotherapy or in conjunction with itraconazole but it has more side effects, especially in cats that are more susceptible to iodism.
- Treat for 4 to 8 weeks post clinical resolution. Median treatment durations is 4 months.
- Cats are at higher risk to transmit the disease to people because they carry large numbers of yeast organisms in the exudate from lesions.
- Make sure to wear disposable gloves when handling any cat with draining lesions and wash hands and arms after handling the disease animal.
- Decontaminate cages and animal carriers and properly disinfect the surfaces where the affected animal contacted.
References
Barrs VR, Bęczkowski PM, Talbot JT et al. Invasive fungal infections and oomycoses in cats. 1. Diagnostic approach. J Fel Med Surg 2024; doI: 10.1177/1098612X231219696
Barrs VR, Hobi S, Wong A et al. Invasive fungal infections and oomycoses in cats. 2. Antifungal therapy. J Fel Med Surg 2024; doI: 10.1177/1098612X231220047
de Lima Barros MB, de Almeida Paes, Schubach AO. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev 2011; 24: 633-654.
de Souza CP, Lucas R, Ramadinha RHR et al. Cryosurgery in association with itraconazole for the treatment of feline sporotrichosis. J Fel Med Surg 2015; DOI: 10.1177/1098612X15575777
Greene CE. Infectious Diseases of the Dog and Cat. 4th ed. St. Louis, Missouri, Elsevier, Saunders, 2012.
Gremiao IDF, da Silva da Rocha EM, Montenegro H et al. Guidelines for the management of feline sporotrichosis causes by Sporothrix brasiliensis and literature review. Braz J Microbiol 2020; DOI: 10.1007/s42770-020-00365-3
Hoffmann AR, Ramos MG, Walker RT et al. Hyphae, pseudohyphae, yeasts, spherules, spores, and more: A review on the morphology and pathology of fungal and oomycete infections in the skin of domestic animals. Vet Pathol 2023; doi.org/10.1177/03009858231173715
Miller WH, Griffin CE, Campbell KL. Muller & Kirk’s Small Animal Dermatology. 7th ed. St. Louis, Missouri, Elsevier, Mosby, 2013.
Reis EG, Schubach TM, Pereira SA et al. Association of itraconazole and potassium iodide in the treatment of feline sporotrichosis: a prospective study. Med Mycol 2016; doi: 10.1093/mmy/myw027
Rippon JW. Medical Mycology. Philadelphia, WB Saunders, 1988.
Rodrigues AM, Della Terra PP, Gremiao ID et al. The threat of emerging and re-emerging pathogenic Sporothrix species. Mycopathologia 2020; 185: 813-842.
Santos AF, Azevedo MI, Amaral CI et al. Feline sporotrichosis: Characterization of cutaneous and extracutaneous lesions using different diagnostic methods. Vet Pathol 2024; 6: 221-231.
Scott DW. Large Animal Dermatology. Philadelphia, WB Saunders, 1988.

