2.10 Otitis Externa – Dogs and Cats
Learning Objectives
- Remember! Otitis externa is a symptom of many diseases, not a specific diagnosis. It may be present in as many as 10% to 20% of the dogs brought to a small animal hospital. To successfully manage otitis externa, it is important for the clinician to identify all of the factors contributing to the ear disease.
- Know the primary, predisposing, and perpetuating causes of otitis externa.
- Learn the clinical signs associated with otitis externa.
- Learn how to diagnose otitis externa.
- Know how to manage otitis externa.
- Remember! RECHECK otitis cases until complete resolution of the problem.
- Know when systemic antibiotic therapy is indicated to manage otitis.
- Know the protocol used for long-term management of allergic otitis.
- Know how to manage chronic hyperplastic otitis.
- Know the drugs that can be potentially ototoxic and should be avoided.
- Otitis media is a common perpetuating factor in cases of chronic otitis externa.
-
General Considerations
- Otitis externa is defined as inflammation of the external auditory canal, which mostly but not always is associated with bacterial infection or Malassezia and/or bacteria overgrowth.
- Otitis externa may be present in as many as 10% to 20% of the dogs brought to a small animal practice.
- In cats, otitis externa is less common than in dogs and is most often related to a parasitic etiology (i.e. Otodectes cynotis otitis) or inflammatory polyps.
- A recently adapted classification scheme divides the factors contributing to ear disease into those that are primary, secondary, predisposing, and perpetuating.
- To successfully manage otitis externa it is important for the clinician to identify these factors (see below).
Important Facts
- Otitis externa is an inflammation of the external ear canal often associated with bacterial infection or Malassezia and/or bacterial overgrowth.
- It may account for 10 to 20% of the dogs brought to a small animal practice.
- It is less common in cats.
- To successfully manage otitis externa, the primary, secondary, predisposing and perpetuating factors contributing to the ear disease need to be identified by the clinician.
-
The Factors
- Primary Factors: Primary factors are those that can directly cause otitis externa. They can produce otitis externa alone without the presence of secondary, predisposing or perpetuating factors.
- Parasites:
- Otodectes cynotis causes approximately 50% of otitis externa in cats and 5 to 10% in dogs. Dogs and cats can be asymptomatic carriers.
- Parasites:
- Primary Factors: Primary factors are those that can directly cause otitis externa. They can produce otitis externa alone without the presence of secondary, predisposing or perpetuating factors.



-
-
-
- Otodectes cynotis mites can also be present outside the ear canals.
- Demodex sp mites can cause a ceruminous otitis in dogs and cats.
- Ticks and chiggers can rarely be found in the ear canals and be the cause of otitis externa in dogs and cats.
- Foreign Bodies:
- It is usually unilateral.
- Look for plant awns, dirt, sand, small stones, impacted wax, loose hair, dried medication.
-
-

-
-
-
- The inciting foreign body may never be identified, especially if small, because it can become completely coated with cerumen.
- Failure of Epithelial Migration:
- A defect in epithelial migration may be responsible for the accumulation of wax and keratin in the ear canal leading to the formation of soft wax plugs, hard concretions or ceruminoliths.
-
-


-
-
-
- Ceruminoliths can cause discomfort leading to head shaking and rubbing, hearing deficits and secondary yeast and bacteria ear infections.
- If ceruminoliths are attached to the tympanum, material may be released into the middle ear leading to otitis media (Refer to Otitis Media).
- Hypersensitivities:
- Atopic Dermatitis – Environmental-induced or food-induced atopic dermatitis
- Otitis externa is seen in 50% to 80% of atopic dogs and in 3 to 5 % of these dogs, the otitis is the only symptom present.
- Atopic Dermatitis – Environmental-induced or food-induced atopic dermatitis
-
-


-
-
-
-
- Atopic dermatitis is the most common cause of persistent or recurrent otitis externa in dogs.
- Initially the disease is characterized by mild to moderate erythema of the inner pinnae and vertical canals.
- Chronic inflammation leads to proliferative changes and to secondary bacteria and yeast infections.
-
- Keratinization Disorders:
- Breeds prone to have idiopathic primary seborrhea (e.g. American cocker spaniels), tend to have otitis externa.
- The keratinization disorders generally present as chronic ceruminous otitis externa (i.e. erythroceruminous otitis).
-
-

-
-
-
- Sebaceous adenitis may present with dry and scaly ears with mild to moderate inflammation.
-
-

-
-
-
- Animals with keratinization disorders usually have other skin involvement.
- Endocrine Diseases:
- Endocrinopathies such as hypothyroidism, hyperadrenocorticism, and sex hormone imbalances may result in chronic ceruminous otitis externa, possibly by altering keratinization and glandular function. However, these are uncommon to rare primary causes of otitis externa with hypothyroidism being the disease reported more frequently.
- In cases of endocrinopathies associated with otitis externa, the animal will present with systemic signs and other cutaneous signs.
- Immune-mediated:
- Lesions of juvenile cellulitis often develop on the pinnae and extend to the ear canals, causing otitis externa.
-
-

-
-
-
- Other body sites such as the muzzle and periocular regions are typically affected. Submandibular (especially) and pre-scapular lymphadenopathy is the disease hallmark.
-
-

-
-
-
- Obstructive ear diseases
- Inflammatory Polyps:
- Polyps are a common cause of otitis externa in cats and less commonly seen in dogs.
- They may originate from the epithelium lining of the tympanic cavity, auditory (Eustachian) tube, or nasopharynx.
- Inflammatory Polyps:
- Obstructive ear diseases
-
-

-
-
-
-
- Feline ceruminous or apocrine cystadenomatosis or ceruminous glands cystomatosis:
- Cats with this condition develop multiple cysts of the ceruminous (apocrine) glands present at the pinnae, external ear canals and preauricular area. In some cats, the apocrine glands present in the eyelids, perioral and perianal regions are also affected.
- Feline ceruminous or apocrine cystadenomatosis or ceruminous glands cystomatosis:
-
-
-

-
-
-
-
- Feline proliferative necrotizing otitis externa:
- It is a rare disease associated with proliferation and necrosis of the ear canal and pinna tissues. Young cats (2-8 months) are typically affected.
- Feline proliferative necrotizing otitis externa:
-
-
-

-
-
-
-
- Neoplasia:
- Dogs: Examples of aural tumors affecting the external ear canal reported in dogs include ceruminous gland adenoma and adenocarcinoma, squamous cell carcinoma, papilloma, histiocytoma, basal cell tumor, sebaceous gland adenoma, plasmacytoma, soft tissues sarcoma, and melanoma.
- Neoplasia:
-
-
-


-
-
-
-
-
- Cats: The most common neoplasia of the external ear canal reported in cats include squamous cell carcinoma, ceruminous gland adenoma and adenocarcinoma, sebaceous gland adenoma or carcinoma.
- Aural tumors tend to be more aggressive in cats than dogs.
- Cats: The most common neoplasia of the external ear canal reported in cats include squamous cell carcinoma, ceruminous gland adenoma and adenocarcinoma, sebaceous gland adenoma or carcinoma.
-
-
-
-
Important Facts
- Primary factors are those that can directly cause the otitis externa.
- The most common primary factors seen in a dermatology referral practice are hypersensitivity disorders and feline ear mites.
- Otitis externa is seen in 50% to 80% of dogs with environmental-induced or food-induced atopic dermatitis and in 3 to 5 % of these dogs, otitis is the only symptom that they have.
- Atopic dermatitis (environmental or food induced) is the most common cause of persistent or recurrent otitis externa in dogs.
- Idiopathic primary seborrhea can present with chronic ceruminous otitis externa especially in the American cocker spaniel.
- The best example of the immune-mediated category is juvenile cellulitis because very often the pinnae and external ear canals are affected.
- Inflammatory polyp (common in cats) and neoplasia are some examples of obstructive ear disease.
-
- Secondary Factors:
- Secondary factors cause disease in an ear canal that is already abnormal.
- They aggravate the clinical signs associated with primary factors.
- Secondary factors, or causes, are typically easy to identify but can be challenging to eliminate.
- Infectious causes:
- Bacteria (e.g. Staphylococcus pseudintermedius, Pseudomonas aeruginosa, Proteus mirabilis, Enterococcus spp., Escherichia coli, Corynebacterium spp. etc).
- Secondary Factors:
-
-
-
- Yeast (e.g. Malassezia spp) or filamentous fungus (e.g. Aspergillus etc).
-
-
-
-
- Iatrogenic:
- Topical medications and ear cleaners can result in an irritant or allergic reaction.
- When otitis externa worsens after proper treatment initiation, consider the possibility of post-treatment contact allergy or irritant dermatitis.
- Iatrogenic:
-

-
-
-
- Trauma or irritation from inappropriate use of cotton swabs or cotton tips.
-
-

Important Facts
- Secondary factors cause disease in an ear canal that is already abnormal.
- They aggravate the primary factor or cause.
- They are typically easy to identify but can be challenging to manage.
- Secondary factors include bacterial infection or bacterial and yeast overgrowth and iatrogenic irritation.
- Once predisposing and/or primary factors cause alterations in the ear canal’s structure and function, bacteria may multiply unchecked.
-
- Predisposing Factors: Predisposing factors alone may not cause otitis externa, but they increase the risk for the development and persistence of secondary causes.
- Ear canal anatomy and conformation:
- Cocker and springer spaniels have shown in a study to have more ceruminous glands and hair follicles in their ear canals than greyhounds and mongrels.
- Ear canal anatomy and conformation:
- Predisposing Factors: Predisposing factors alone may not cause otitis externa, but they increase the risk for the development and persistence of secondary causes.

-
-
-
- Stenotic ear canals: Shar Pei, Chow chow, and brachycephalic breeds (e.g. pugs, American and French bulldogs) have narrower horizontal canals than dolichocephalic breeds.
-
-


-
-
-
- Hairs in external ear canals (e.g., poodle) and large pendulous pinnae (e.g., Basset hound) can prevent normal aeration and promote debris accumulation in the canals.
-
-


-
-
- Maceration of the ear canal from excessive moisture:
- Moisture accumulation in the ear canals from bathing or swimming or excessive ear cleaning.
- Maceration of the ear canal from excessive moisture:
-

Important Facts
- Predisposing factors alone may not cause otitis externa, but they increase the risk for development and persistence of secondary factors.
- Predisposing factors include factors related to the ear canal anatomy and conformation and maceration of the ear canal epithelium from excessive moisture.
-
- Perpetuating Factors: They are capable of perpetuating the otitis even if the primary factor has been removed.
- Chronic pathologic changes: these changes lead to alteration in the anatomy and physiology of the ear canal in response to chronic and recurrent otitis externa.
- Inappropriate treatment can eventually lead to perpetuation of the otitis externa.
- With chronic inflammation, the epidermis, dermal glands and fibers and subcutis tissue proliferate excessively leading to stenosis of the ear canal.
- The auditory cartilages may eventually undergo calcification and ossification, which is more often seen in cocker spaniels and bulldogs with chronic otitis externa.
- Calcified ear canal tissues are permanent changes that cannot be resolved with medical treatment.
- This disease stage is called “end stage otitis” and total ear canal ablation and bulla osteotomy is recommended (TECABO).
- Chronic pathologic changes: these changes lead to alteration in the anatomy and physiology of the ear canal in response to chronic and recurrent otitis externa.
- Perpetuating Factors: They are capable of perpetuating the otitis even if the primary factor has been removed.

-
-
-
- With chronic and recurrent inflammation, the ear self-cleaning mechanism is disrupted leading to failure of the ear canal epithelium to migrate outwards. This epithelial migration is important for the elimination of microorganisms, dead epithelial cells, glandular secretion and debris.
- Secretions, desquamated cells, and proliferating microorganisms become entrapped with abnormal epithelium migration.
- Chronic otitis externa often results in extension of the disease into the middle ear leading to chronic otitis media (Refer to Otitis Media).
- With chronic and recurrent inflammation, the ear self-cleaning mechanism is disrupted leading to failure of the ear canal epithelium to migrate outwards. This epithelial migration is important for the elimination of microorganisms, dead epithelial cells, glandular secretion and debris.
-
-
Important Facts
- Perpetuating factors are factors capable of perpetuating the otitis even if the primary factor has been removed.
- Perpetuating factors include the factors that eventually lead to chronic pathologic changes in the external ear canals such as, hyperplasia and calcification.
- Calcified ear canal tissues are permanent changes that cannot be resolved with medical treatment.
- Chronic otitis externa often results in extension of the disease into the middle ear leading to chronic otitis media.
-
Clinical Signs
- Clinical signs of otitis externa are quite variable and will depend on the following:
- Underlying primary disease – Examples: otitis caused by Otodectes cynotis infestation tends to be very itchy; otitis associated with juvenile cellulitis has nodules, papules and tends to be very exudative etc.
- Presence of secondary problems and their nature (see type of discharge below)
- Duration and extent of the problem – if the otitis becomes chronic, hyperplasia and eventually calcification of soft tissues will occur.
- The type of discharge may be a clue as to which infectious agent may be involved. However, always perform cytology!!!!
- Debris resembling dry coffee grounds is typical of otitis caused by Otodectes cynotis mites. Careful otoscopic examination may allow for visualization of the mites as they move within the canal.
- Yellow to tan waxy/greasy discharge is usually associated with cocci but it can sometimes be a sign of Malassezia spp. overgrowth.
- Clinical signs of otitis externa are quite variable and will depend on the following:

-
-
- Black and moist discharge is typically seem with Malassezia spp. overgrowth.
-

-
-
- Purulent creamy to yellow exudate is most often seen with gram-negative infections, such as Pseudomonas aeruginosa and Proteus spp.. Pseudomonas aeruginosa is also associated with very inflamed, eroded to ulcerated ear canals. Pain is also a common sign.
-

-
- In chronic cases, the epithelial lining of the ear canal will often evidence a cobblestone appearance.
- In severe longstanding cases of otitis externa, stenosis and ossification of the cartilage and soft tissue of the external ear canal may occur.
- Calcification is seen more often in American cocker spaniels and bulldogs and is known as end-stage otitis.
- In chronic cases, the epithelial lining of the ear canal will often evidence a cobblestone appearance.
Important Facts
- The type of discharge may be a clue as to which infectious agent may be involved. However, always perform cytology!!!!
- Debris resembling dry coffee grounds is typical of ear mites.
- Yellow to tan waxy/greasy discharge is usually associated with cocci but it can sometimes be a sign of Malassezia spp. overgrowth.
- Black and moist discharge is typically seem with Malassezia spp. overgrowth.
- Purulent creamy to yellow exudate is most often seen with gram-negative infections such as Pseudomonas aeruginosa and Proteus spp.. Pseudomonas aeruginosa is also associated with very inflamed, eroded to ulcerated and painful ear canals.
- In chronic cases, the epithelial lining of the ear canal will often evidence a cobblestone appearance.
- In severe longstanding cases of otitis externa, ossification of the cartilage and soft tissue of the external ear canal may occur.
-
Diagnosis
- History and Physical Exam:
- A thorough history and physical examination are fundamental diagnostic procedures. They will help with the identification of the factors.
- Diagnosis of deafness might be based on owner and veterinarian assessments; however, Brainstem Auditory Evoked Response (BAER) may be performed to confirm deafness and detect unilateral or bilateral hearing deficits. BAER may also be used to monitor progressive changes in hearing over time.
- History and Physical Exam:


-
-
- Examine the face/head for evidence of facial nerve paralysis (i.e. ipsilateral drooping or inability to move ear or lip, drooling, decrease or absent palpebral reflex) or Horne’s syndrome (i.e. protrusion of the third eyelid, ptosis, narrowing of the eye opening, sunken eye appearance and miosis. These signs may indicate middle ear disease. Signs of inner ear disease include head tilt, nystagmus and peripheral vestibular ataxia.
-


-
-
- Examine the oral cavity for evidence of pain when opening the mouth (may indicate severe otitis media), inflammation, and masses (e.g. nasopharyngeal polyps in cats).
- Examine the pinna and entrance of the external ear canal. Palpate the upper portion of the cartilage of the vertical ear canal for presence of pain, thickening, excess exudate, and calcification.
- Perform a hand-held otoscopic examination or, if available, a video otoscope examination to assess presence and degree of inflammation, stenosis, proliferative changes, amount and nature of debris and discharge, presence of foreign bodies, ectoparasites, masses and integrity of tympanic membrane.
-


-
-
- Sedation or/and anesthesia may be necessary to perform a thorough otoscopic examination.
- If the ear canal is extremely inflamed, swollen, and stenotic, it is best to start treatment to reduce inflammation and then examine the canal at a later visit.
-
Important Facts
- A thorough dermatologic history and physical examination are fundamental diagnostic procedures.
- Examine the face for evidence of middle ear (ipsilateral drooping or inability to move ear or lip, drooling, decrease or absent palpebral reflex, exposure keratitis) and inner ear (head tilt, nystagmus, ataxia) involvement.
- Examine oral cavity for evidence of pain when opening the mouth (severe otitis media), inflammation, and masses (especially nasopharyngeal polyps in cats).
- Examine the pinna and entrance of external canal and palpate ear cartilage for the presence of pain, thickening, excess exudate, and calcification.
- Perform a hand-held otoscopic examination or a video otoscope examination if available.
-
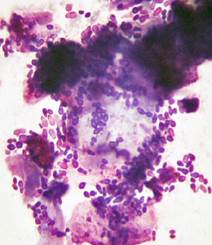
- Cytology: This is necessary not an option!
- Take one swab for Otodectes cynotis mites or Demodex mites and place the sample on a glass slide with mineral oil.
- Take another swab for cytology and stain it with Diff Quik or another Romanowsky stain. Examine the stained slide under immersion oil.
- Cytology: This is necessary not an option!


-
-
- Record the presence of cocci-shaped bacteria, usually Staphylococcus spp., and rod-shaped bacteria, usually Pseudomonas spp.). Also, record the presence of yeast, usually Malassezia spp.
- If large numbers of degenerate neutrophils, red blood cells and rod-shaped bacteria are present, be highly suspicious of Pseudomonas otitis.
- Repeat cytology at each recheck visit! You want to know if you are making progress or if new agents are present.
- If infection persists in face of treatment, it suggests inappropriate treatment, resistance or poor owner compliance.
- If inflammatory cells persists but no bacteria or yeast are seen, it suggests that an irritant reaction otic medications or cleansers is present.
- When treating Pseudomonas otitis, neutrophils may persist on cytology long after the infection is resolved indicating that the erosive to ulcerative lesions are not completely healed.
- Record the presence of cocci-shaped bacteria, usually Staphylococcus spp., and rod-shaped bacteria, usually Pseudomonas spp.). Also, record the presence of yeast, usually Malassezia spp.
-
Important Facts
- Take one swab for Otodectes cynotis mites or Demodex mites and place the sample on a glass slide with mineral oil.
- Take another swab for cytology, stain the sample with Diff Quik, and examine under mineral oil immersion.
- Repeat cytology at each recheck visit!
- If organisms persist on cytology in face of treatment, it suggests inadequate treatment, resistance or poor owner compliance.
- If inflammatory cells persists on cytology but no bacteria or yeast are seen, it suggests that an irritant reaction to medications is present.
- When treating Pseudomonas otitis neutrophils may persist on cytology long after the infection is resolved indicating that the ulcerative lesions are not completely healed.
-
- Bacterial Culture and Sensitivity:
- The need for performing bacterial culture and susceptibility is controversial at this time.
- The rationale for not performing bacterial culture and susceptibility is because the local concentration of the antibiotic surpasses the drug in vitro MIC (minimal inhibitory concentration) by a factor as high as 100 times. Thus, the antibiotic should be effective even when resistant in vitro. In addition, the available in vitro tests are based on serum concentration of the antibiotic not tissue concentration.
- Very little studies have been done in vivo to test this concept.
- Until more studies are done, the authors recommend performing bacterial culture & susceptibility in the following circumstances.
- Every time gram-negative rods are seen on cytological examination.
- Presence of gram-negative rods on cytology usually indicate Pseudomonas aeruginosa and less commonly Proteus spp.
- Both organisms produce biofilm and develop resistance to antibiotics very easily.
- Every time gram-negative rods are seen on cytological examination.
- The need for performing bacterial culture and susceptibility is controversial at this time.
- Bacterial Culture and Sensitivity:
-
-
-
- When bacteria are seen on cytological examination despite appropriate topical therapy.
- Chronic refractory or recurrent cases or cases with history of resistant infections.
- When otitis media has been diagnosed and systemic therapy has been considered as part of the treatment regimen.
-
-
Important Facts
- The need for performing bacterial culture and sensitivity is controversial at this time.
- The authors recommend performing bacterial culture and susceptibility in the following circumstances: (i) every time gram-negative rods are seen on cytological examination; (ii) when bacteria are seen on cytological examination despite appropriate topical therapy; (iii) chronic refractory or recurrent cases or cases with history of resistant infections; and (iv) presence of otitis media.
-
- Imaging – CT scan or MRI
- CT scan or MRI is mainly indicated in the workup of chronic or recurrent otitis externa to assess the degree of bulla involvement when otitis media is suspected.
- Advanced imaging is very sensitive; however, false negative results are possible.
- MRI is best for the assessment of soft tissue changes and the diagnosis of otitis interna but it is more expensive.
- CT scan is best for assessment of bone structures thus it is best used for the diagnosis of otitis media.
- Radiographs are not very sensitive and approximately 25% of otitis media cases in dogs and cats have no radiographic changes.
- CT scan or MRI is mainly indicated in the workup of chronic or recurrent otitis externa to assess the degree of bulla involvement when otitis media is suspected.
- Imaging – CT scan or MRI


Important Facts
- CT scan is best for assessment of bone structures and is best used for the diagnosis of otitis media.
- MRI is best for the assessment of soft tissue changes and the diagnosis of otitis interna but it is more expensive.
- Radiographs are not very sensitive and approximately 25% of otitis media cases in dogs and cats have no radiographic changes.
-
- Biopsy:
- Tissue biopsy is performed to collect samples of masses present in the ear canals.
- Using the correct instrument is very important to obtain proper samples.
- Alligator forceps or loops are often used but they can only collect small samples, so take multiple samples and try to reach the core of the lesion. These instruments pass through the operating channel of the video otoscope.
- Biopsy:



-
-
- Be mindful that the wrong diagnosis may be given if the lesion is large or bulky and the core of the lesion cannot be sampled.
-
Important Facts
- Tissue biopsy is performed to collect samples of masses present in the ear canals.
- Using the correct instrument is very important to obtain proper samples.
- Be mindful that the wrong diagnosis may be given if the core of the lesion cannot be sampled
-
Treatment
- Successful treatment means identifying and resolving or controlling the primary, secondary, and predisposing factors or causes, if possible.
- Perpetuating factors associated with chronic otitis should be ideally prevented but if present, proper treatment to restore the anatomic and functional abnormalities should be instituted.
- Cleaning and drying of the ear canal and topical therapy are part of the treatment regimen and should be tailored to each patient.
- In-Hospital Ear Cleaning:
- To assure that the ear canals are free of discharge and debris prior to topical treatment, it is recommended that the clinician or experienced technician perform the initial cleaning.
- Products containing the following ingredients should be avoid or used carefully if the tympanic membrane is ruptured or its status is unknown:
- Chlorhexidine, propylene glycol, alcohol-containing products, acetic acid and ceruminolytics with the exception of squalene (see “At-home Ear Cleaning for more detail on ceruminolytics).
- There is some evidence that ≤ 0.05% chlorhexidine solutions may be safe in the middle ear.
- Ears with minimal discharge and patent canals may be cleaned without sedation.
- The status of the tympanic membrane should be established before cleaning.
- Sedation may be needed in some cases.
- If the tympanic membrane cannot be visualized due to excessive discharge or debris, or if it is known to be ruptured, saline can be used to rinse the ear.
- If an animal swallows, gags, or coughs when fluid is placed in the ear, it is a good indication that the tympanic membrane is ruptured.
- If saline is not able to rinse away the discharge or debris than a solution containing squalene can be safely used. However, it should be realized that there is no completely safe solution for cleaning the middle ear.
- If the tympanic membrane is intact, solutions containing an ototoxic ceruminolytic (e.g. dioctyl sodium sulfosuccinate, carbamide peroxide, triethanolamine etc.) can be applied inside the ear canal.
- The ear canal is then massaged for 1 to 2 minutes to loosen and dissolve the discharge and debris and the excess solution and debris that has floated to the surface is wiped away with a cotton ball.
- The ear canal is then flushed with lukewarm water using a bulb syringe to removed residue of these ear cleaners.
- Failure to rinse these solutions from the ear canals may result in irritation to the epithelium of the ear canal.
- If suction is available, attach it to a No. 8-Fr urinary catheter cut to a length of about 15 cm, and suction any remaining water and debris from the ear canal while observing through an operating head otoscope. Thereafter, examine the canal to verify that it is completely clean and, if not, repeat the process.
- In chronic and recurrent cases, video otoscopy under anesthesia is the ideal method to thoroughly clean and assess the external ear canal and tympanic membrane integrity. Advanced imaging (i.e. CT scan or MRI) is also recommended before the video otoscopic procedure to evaluate the middle ear.
- Successful treatment means identifying and resolving or controlling the primary, secondary, and predisposing factors or causes, if possible.
Important Facts
- Successful treatment means identifying and resolving or controlling the primary, secondary, predisposing and perpetuating factors or causes, if possible.
- Cleaning and drying of the ear canal and topical therapy are part of the treatment regimen and should be tailored to each patient.
- It is recommended that the clinician or experienced technician perform the initial cleaning.
- In chronic cases, video otoscopy under anesthesia is the ideal method to thoroughly clean and assess the external ear canal and tympanic membrane integrity.
- Advanced imaging (i.e. CT scan or MRI) is also recommended before the video otoscopic procedure to evaluate the middle ear.
- Avoid or use carefully products containing chlorhexidine, propylene glycol, alcohol-based products, and ceruminolytics, with the exception of squalene.
- It should be realized that there is no completely safe solution for cleaning the middle ear.
-
- At-Home Ear Cleaning:
- Periodic cleaning by the owner is often necessary to remove the excessive discharge associated with continued inflammation or infection.
- It is important to demonstrate the cleaning procedure at least one time to the client.
- The owner is instructed to instill the cleaning solution into the ear canal until it starts to spill out. If needed, some of the cleansing liquid can be rubbed on the ear pinnae.
- The upper portion of the cartilage of the vertical canal is grasped at the base of the ear and the ear canal is gently squeezed and massaged. This is continued for 1 to 2 minutes.
- After the pet shakes its head, loose debris is removed from the ear pinna and entrance to the ear canal with a dry cotton ball, which is used only to clean debris from those areas of the ear that can clearly be seen. This procedure is repeated until the cotton ball comes out clean.
- Remember to tell pet owners to not introduce cotton swabs in the ear canals to avoid packing of the discharge deep in the canal.
- It is recommended to clean the ears of dogs with atopic dermatitis at least once weekly for their lives, as these animals are prone to develop ear infections and atopic dermatitis is a non-curable disease.
- The frequency of the cleaning will vary from daily to weekly or longer, depending on the rate of accumulation of discharge or wax in the ear canal.
- For removal of waxy debris, ceruminolytic agents containing dioctyl sodium sulfosuccinate (DSS), carbamide peroxide, triethanolamine, hexamethyletracosane, docusate sodium, calcium sulfosuccinate, or squalene should be used.
- A study tested the effect of squalene, DSS, propylene glycol, carbamide peroxide and triethanolamine in the ear apparatus of dogs and guinea pigs after 4 weeks of treatment. Based on brain auditory evoked response (BAER) test and neurologic examination only squalene caused no morphologic or neurologic abnormality.
- With the exception of squalene, ceruminolytic agents should be avoided in the middle ear and in cases of unknown status or ruptured tympanic membrane.
- Removal of a moist discharge from the ear canal can be accomplished by cleaning with products containing acidic ingredients and/or alcohol.
- Examples of some ingredients in this category include salicylic acid, acetic acid, lactic acid, boric acid, benzoic acid, malic acid and isopropyl or benzyl alcohol.
- Keep in mind that alcohol-containing products are potentially ototoxic.
- Very little is known about the ototoxicity effect of acidic solutions but acetic acid has been listed as “potentially ototoxic” in textbooks. The authors have carefully used acid-containing products in dogs with ruptured tympanic membrane without any problem
- Be mindful that most of the commercial products containing the acid ingredients listed above also contain propylene glycol and should be avoided or used carefully if the tympanic membrane is ruptured or its status is unknown.
- Propylene glycol is known to cause inflammation in the external ear canal but it can also cause inflammation in the mucoperiosteum resulting in the formation of excessive granulation tissue and bony changes in the bulla.
- Examples of some ingredients in this category include salicylic acid, acetic acid, lactic acid, boric acid, benzoic acid, malic acid and isopropyl or benzyl alcohol.
- Tris-EDTA (tris-ethylene diamine tetra-acetic acid) has an antimicrobial potentiating effect. It disrupts the bacterial cell wall of gram-negative bacteria such as, Pseudomonas spp., by chelating ions and making the cell membrane porous allowing the antibiotic to penetrate the bacteria cell wall more effectively.
- There are quite a few ear cleaning products containing Tris-EDTA.
- These products are a good option for patients with Pseudomonas otitis.
- Products containing Tris-EDTA work best if applied 15-30 minutes before the topical antibiotic.
- Some ear cleaning solutions will have ketoconazole and should be selected as part of the treatment regimen of Malassezia otitis.
- At-Home Ear Cleaning:
Important Facts
- It is very important that you demonstrate to the client how to clean the pet’s ear canals.
- Choose the cleaning solution according to the characteristic of the discharge and the severity of the inflammatory process.
- If the ear canals are eroded or ulcerated (often seen with Pseudomonas sp. infections), do not use acidic solutions because they will cause more pain and may aggravate the inflammation.
- The frequency of cleaning will depend on the severity of the condition. In most cases, start with once daily cleaning and reduce to find the ideal maintenance frequency.
- Animals with atopic dermatitis should have their ears cleaned on a long-term basis, at least once weekly.
- Avoid using ceruminolytics (exception squalene), propylene glycol and alcohol containing products in the ear canals if the tympanic membrane is ruptured or its integrity is unknown.
- The potential ototoxic effect of acidic solutions in dogs and cats is currently unknown. However, acetic acid is listed as “potentially ototoxic” in some textbook sources but there is currently no scientific evident to support this claim.
- Ear cleaning solutions containing Tris-EDTA are good options for patients with Pseudomonas otitis and are more effective if used 15-30 minutes before the application of the topical antibiotic.
- Ear cleaning solutions containing ketoconazole should be selected for the treatment of Malassezia otitis.
-
- Antimicrobial-containing Topical Therapies:
- Independent of the condition being treated (i.e. bacterial, yeast or fungal infection or overgrowth), we recommend the following:
- Treat twice daily until the recheck appointment!
- If using the long acting products such as, Claro® or Osurnia®, follow the label recommendation regarding the frequency of administration.
- If treating Pseudomonas otitis, continue treatment for 1 to 2 weeks after a negative cytology and ear culture (refer to previous discussion on ear culture and sensitivity).
- Educate clients to discontinue treatment and contact you immediately, if the ears become redder and/or develop lesions (e.g. papules, vesicles, edema etc) during treatment as these signs could indicate a drug reaction.
- Bacterial infections:
- If doublets or packets of gram-positive cocci are present, it is most likely to be Staphylococcus spp. and topical preparations containing chloramphenicol, aminoglycoside, polymixin B, or fluoroquinolone can be used. Despite the fact that the product will be used locally, practice antibiotic stewardship and select an antibiotic in tier one first, if possible.
- If chains of gram-positive cocci are present, it is most likely to be Streptococcus spp. and a topical preparation containing one of the penicillins would be appropriate.
- If gram-negative rods, degenerate neutrophils and ± red blood cells are present, it is most likely to be Pseudomonas spp. and preparations containing one of the following antibiotics known to be effective against Pseudomonas organisms would be appropriate.
- However, we recommend that the antibiotic be selected based on culture and sensitivity results (refer to previous discussion on ear culture and sensitivity).
- Keep in mind that some of the antibiotics listed below are manufactured as injectable products; however, they can be used topically. Consult a pharmacist or a reliable compounding pharmacy for adequate preparation of the product.
- Only use systemic therapy if the patient has confirmed otitis media, in which case a middle ear sample should be collected for bacterial culture and sensitivity and proper antibiotic selection.
- Antibiotics typically effective for Pseudomonas otitis:
- Gentamicin
- Polymxyxin B
- Amikacin
- Enrofloxacin or another fluoroquinolone
- Silver sulfadiazine
- Ticarcillin
- Ceftazidine
- Independent of the condition being treated (i.e. bacterial, yeast or fungal infection or overgrowth), we recommend the following:
- Antimicrobial-containing Topical Therapies:
Important Facts
- The macroscopic characteristic of the ear exudate can suggest the type of infection present. Nevertheless, always perform cytology to help identify the organisms causing the infection.
- If the cytologic test shows gram negative rods + degenerated neutrophils and ± red blood cells, CULTURE, CULTURE and CULTURE! It is very likely to be Pseudomonas spp. infection and this organism has the capability of developing resistance to antibiotics very easily.
- Only stop therapy when managing Pseudomonas spp. cases after obtaining a negative cytology and culture.
- No matter what infection you are managing, the medication should be applied inside the ear canals at least twice daily — if not using long-acting products — and until resolution.
- Only use systemic antibiotic if a diagnosis of otitis media has been confirmed. In this case, a sample for bacterial culture and sensitivity has to be collected from the middle ear for proper antibiotic selection.
- RECHECK your otitis cases as many times necessary to resolve an episode.
-
-
- Malassezia infections:
- Effective topical active ingredients include:
- Clotrimazole
- Posaconazole
- Miconazole
- Cuprimyxin.
- Effective topical active ingredients include:
- Malassezia infections:
-
Important Facts
- Systemic treatment with ketoconazole, itraconazole or terbinafine can be added to the topical therapy to manage severe and difficult cases of Malassezia otitis.
- Treat until no organisms are identified on cytology.
- Recommend applying the medication twice daily until the recheck visit, if not using long-acting products.
- Perform cytology and an otoscopic examination at all recheck visits.
- Educate the pet owner to discontinue treatment and contact you immediately if the ears become redder than before therapy initiation and develop lesions (i.e. papules, vesicles, edema).
- Identify and treat the underlying disease.
-
-
- Ear mite infestation:
- Fluralaner (Bravecto®): Oral (dogs) or topical (cats) fluralaner at the dose of 25 mg/kg administered to dogs once has shown in a study to eliminate all ear mites after 28 days of therapy. In the same study, cats were treated also once with topical fluralaner at the dose of 40 mg/kg and no mites were seen after 14 days of therapy.
- Another study showed that sarolaner administered at a single dose of 2.0 mg/kg to eight dogs with experimentally-induced Otodectes cynotis otitis led to a reduction of pre-treatment mite count of 98.2%. Another group of eight dogs was treated with two doses at 30 days interval and the mite count reduction was 99.5%.
- Other isoxazolines such as afloxalaner (NexGard) and lotilanar (Credelio) may also be effective but no studies have been published at this time.
- Ivermectin at the dosage of 0.3 mg/kg PO weekly for 3 to 4 weeks or 0.3 mg/kg SQ every 10 to 14 days for 3 treatments have shown to be effective. Clean the excess ear debris with an adequate ear cleaning solution before treatment.
- Fipronil (Top Spot®): Wet a cotton swab with the pour-on product and coat the earflap and ear canal or apply two drops inside each ear canal. Pour the rest of the product on the animal’s dorsum as recommended for flea control. One treatment is usually sufficient; however, recheck the animal in 2 weeks. Clean the excess ear debris with an adequate ear cleaning solution before treatment.
- Revolution® (Selamectin): It has been approved for the treatment of ear mite infestation. It has been reported to be efficacious in the treatment of ear mites with only one application. Clean the excess ear debris with an adequate ear cleaning solution before treatment.
- Regardless of the treatment regimen you choose to manage this condition, treat all in-contact dogs and cats to eliminate mites from asymptomatic carriers.
- Ear mite infestation:
-
Important Facts
- If you are using topical therapy, you should include whole body treatment as art of the regimen because Otodectes cynotis mites can be found in other parts of the body.
- Regardless of the treatment regimen you choose to manage this condition, treat all in-contact dogs and cats to eliminate mites from asymptomatic carriers.
-
-
- Demodicosis:
- Most cases of otic demodicosis will be associated with lesions in various other parts of the body and the treatment used to treat the generalized demodicosis (e.g. isoxazoles, ivermectin, moxidectin etc) will be also effective in treating the otic demodicosis.
- If the demodicosis is localized solely to the ear canals, products with the following active ingredients can be used topically:
- Rotenone
- Amitraz
- Ivermectin
- Thiabendazole
- Demodicosis:
- Topical Anti-inflammatory Therapy:
- Many otic preparations contain glucocorticoids, which will benefit most cases of otitis externa by decreasing inflammation, erythema, pruritus, swelling, exudation, and tissue proliferation.
- Products containing hydrocortisone can be used long-term to control chronic inflammation in patients with atopic dermatitis if used two to three times weekly.
- Be aware! Daily to every-other-day, long-term topical use of glucocorticoids in the ear canal may result in systemic absorption resulting in elevations of liver enzymes and suppression of the adrenal response to adrenocorticotrophic hormone (ACTH).
- Monitor for potential side effects if recommending long-term use of otic products containing glucocorticoids.
- Chronic, Proliferative Otitis:
- The best management for chronic, proliferative or hyperplastic otitis is to prevent it!
- In order to “save” the ear, aggressive medical therapy is needed to reduce the tissue proliferation. Treatment should include:
- Systemic glucocorticoids: Prednisone or prednisolone at the dosage of 0.5 mg/kg q 12h for 2 weeks, then 0.5 mg/kg q 24 h for 2 weeks then 0.5 mg/kg q48 h for 2 weeks or until proliferative changes have greatly improved or resolved.
- Topical glucocorticoid therapy, or in association with systemic glucocorticoids, is critical.
- If the canal is hyperplastic but not calcified, treatment with a solution containing fluocinolone acetonide in 60% dimethylsulfoxide (Synotic®, Syntex Animal Health) can be beneficial mainly if applied 4 to 6 times daily. Recheck the animal in 4 weeks.
- NOTE! Hyperplastic changes rarely return to complete normalcy and long-term maintenance therapy is required. Once the proliferation is controlled, maintenance therapy using the protocol described for “Long-Term Management of Allergic Otitis” (see below) should be instituted.
- Medical therapy will not work for calcified ear canals or end-stage otitis. These cases will require surgery (see below under Indications for Surgery).
-
Important Facts
- The best management for chronic, hyperplastic otitis is to prevent it!
- In order to “save” the ear, aggressive medical therapy is needed to reduce the tissue proliferation.
- Topical glucocorticoid therapy is necessary and it can be used alone or in association with systemic glucocorticoids.
- Treatment with a solution containing fluocinolone acetonide in 60% dimethylsulfoxide (Synotic®) can be very beneficial to reduce the tissue hyperplasia if applied 4 to 6 times daily.
- NOTE! Hyperplastic ears rarely return to complete normalcy and long-term maintenance therapy is required.
- Medical therapy will not work for calcified ear canals or end-stage otitis. These cases will require surgery (i.e. total ear canal ablation and bulla osteotomy (TECABO).
-
- Long-Term Management in Allergic Otitis:
- Clean ears routinely 1 to 2 times weekly or as needed.
- Resolve secondary bacterial and/or yeast overgrowth.
- THEN USE: long-term maintenance therapy with topical glucocorticoid instilled in the ear canals as infrequently as possible to control inflammation primarily associated with the allergic disease.
- REMEMBER! Control of the underlying allergic disease is crucial to the successful treatment of allergic otitis.
- Long-Term Management in Allergic Otitis:
Important Facts
- The long-term management of allergic otitis will involve cleaning the ears once to twice weekly and applying topical glucocorticoid instilled in the ear canals as infrequently as possible to control inflammation.
- The long-term management of allergic otitis will involve cleaning the ears once to twice weekly and applying topical glucocorticoid instilled in the ear canals as infrequently as possible to control inflammation.
- Control of the underlying allergic disease is crucial to the successful treatment of allergic otitis.
-
- Ototoxicity:
- The incidence of ototoxicity in dogs and cats is not known; however, it appears to be rarely observed in practice.
- What we know about ototoxicity is mostly based on anecdotal reports, studies performed in species other than the dog and cat, or on reports where drug concentrations are much higher than what is found in proprietary medications.
- In one study when 0.2% chlorhexidine was placed in the external ear canal of dogs with ruptured tympanic membranes, no signs of ototoxicity occurred.
- In another study, when 0.3% gentamycin was placed twice a day for 21 days in the external ear canals of dogs with experimentally ruptured tympanic membranes, no signs of ototoxicity developed. However, cats may be more sensitive to aminoglycosides.
- It is important, however, to be aware of potentially ototoxic compounds, particularly when the tympanic membrane is not intact or its status is unknown.
- Products reported to be non-ototoxic:
- Aqueous dexamethasone, fluocinolone, ciprofloxacin, enrofloxacin, ofloxacin, penicillin G, carbenicillin, ticarcillin (controversial), ceftazidime, cefmenoxine, miconazole, clotrimazole, nystatin, tonalftate, squalene, triz-EDTA.
- Products reported to be ototoxic:
- Organic acids (salicylic, malic and lactic), detergents and alcohols, chlorhexidine, gentamicin, amikacin, tobramycin, neomycin, polymyxin B and most ceruminolytics.
- The incidence of ototoxicity in dogs and cats is not known; however, it appears to be rarely observed in practice.
- Ototoxicity:
Important Facts
- Ototoxicity is rare in veterinary medicine.
- Veterinarians need to be aware of potentially ototoxic compounds, particularly when the tympanic membrane is not intact or its status is unknown.
-
- Indications for Surgery:
- Vertical ear ablation is an option when a mass is present in the vertical canal but the horizontal canal is not affected.
- Total ear canal ablation and bulla osteotomy (i.e. TECABO) are indicated when there is irreversible proliferation and/or calcification of the auricular cartilages and soft tissues of the vertical and horizontal ear canals and otitis media.
- Because chronicity and severity of the ear disease results in partial to total deafness, ablation does not tend to produce a noticeable increase in hearing difficulties.
- Damage of the facial nerve can occur in as many as 20% of the dogs during surgery.
- This surgery should only be performed by a board certified surgeon.
- Indications for Surgery:
References
Brame B, Cain C. Chronic otitis in cats: Clinical management of primary, predisposing and perpetuating factors. J Feline Med Surg 2021; 23: 433-446.
Bishoff MG, Kneller SK. Diagnostic imaging of the feline and canine ear. Vet Clin North Am: Small Anim Pract 2004; 34(2): 437-558.
Gortel K. Otic flushing. Veterinary Clinics of North America: Small Anim Pract 2004; 34(2): 557-565.
Greci V, Mortellaro CM. Management of otic, nasopharyngeal, and nasal polyps in cats and dogs. Vet Clin Small Anim 2016; 46: 643-661.
Griffin GE, Kwochka KW & Macdonald JM. Diseases of the Ear. In: Current Veterinary Dermatology: The Science and Art of Therapy. Mosby Year Book, St Louis, 1993, p 245-262.
Koch SN, Torres SMF, Plumb DC. Canine and Feline Dermatology Drug Handbook Small 2012. Wiley-Blackwell, Ames, Iowa. p. 369-393.
Morris DO. Medical therapy of otitis externa and otitis media. Vet Clin North Am: Small Anim Pract 2004; 34(2): 541-555.
Njaa BL, Cole LK, Tabacca N. Practical otic anatomy and physiology of the dog and cat. Vet Clin Small Anim 2012; 42: 1109-1126.
Nuttall T. Managing recurrent otitis externa in dogs: what have we learned and what can we do better? J Am Vet Med Assoc 2023; doi.org/10.2460/javma.23.01.0002.
Oishi N, Talaska AE, Schacht J. Ototoxicity in dogs and cats. Vet Clin Small Anim 42 (2012) 1259–1271.
Schuldenfrei MD, Lam AT, Outerbridge CA, et al. Evaluation of aural masses submitted as inflammatory polyps in 20 dogs (2000-2020). Vet Derm 2022; DOI: 10.1111/vde.13123.
Six RH, Becskei Csilla, Mazaleski MM et al. Efficacy of sarolaner, a novel isoxazoline, against two common mite infestations in dogs; Demodex spp. and Otodectes cynotis. Vet Parasitol 2016; 222:62-66.
Taenzler J, de Vos C, Rainer K. A. Roepke RKA et al. Efficacy of fluralaner against Otodectes cynotis infestations in dogs and cats. Parasit Vectors 2017; DOI 10.1186/s13071-016-1954-y.

