1.2 Feline Pyodermas
Learning Objectives
- What does cause feline cutaneous abscess and cellulitis?
- What bacteria are often isolated from cutaneous abscesses in cats?
- How do you manage a case of feline cutaneous abscess or cellulitis (include antibiotic options and duration of therapy)?
- What should you do in resistant cases?
-
General Considerations
- Bacterial folliculitis and deep pyodema are less common in cats than in dogs, but do not underestimate their presence.
- Poor Staphylococcus spp. adherence to feline corneocytes, an important first step for colonization and infection to occur, may explain why this bacterium is less prone to develop skin infections in cats than in dogs and people. In support of this theory, are the findings of a study showing that different species and strains of Staphylococcus adhered significantly less to feline corneocytes than to canine and human corneocytes. Other host factors that may play a role in determining whether bacterial exposure results in transient contamination or infection include differences in epidermal barrier function, local skin microenvironment, and innate or adaptive immune response.
- Abscess/cellulitis due to fight wounds is common in cats.
- The feline skin flora is not well defined. Staphylococcus pseudintermedius (previously S. intermedius) and S. aureus are considered residents. Other species include coagulase negative Staphylococcus spp. (i.e. S. simulans, S. epidermidis, S. xylosus, and S. felis), alpha-hemolytic streptococci and Acinetobacter spp.
- Only feline abscess/cellulitis will be discussed under “Feline Pyodermas”.
-
Abscesses/cellulitis
- Definition:
- Abscess: focal accumulation of pus.
- Cellulitis: diffuse dermal and subcutaneous inflammation that can be sterile or infectious.
- Cause(s):
- Fight wounds caused by the cat’s teeth and claws. During fights, bacteria from the cat’s teeth or claws are introduced into the deep dermis and subcutaneous tissue inducing a walled inflammatory reaction, in the case of an abscess formation, or a diffuse tissue inflammatory response in the case of cellulitis.
- Normal flora of the mouth:
- Anaerobes (Fusobacterium spp, Bacteroides spp, Porphyromonas spp, Peptostreptococcus, Clostridium spp, Prevotella spp).
- Pasteurella multocida.
- B-hemolytic streptococci.
- Staphylococcus spp.
- Escherichia coli.
- Clinical signs:
- Intact males are more often affected.
- Common sites: face, limbs, base of the tail, neck and shoulders.
- Abscess or cellulitis form at the site of the punctured wound. The abscess may rupture and drain a thick purulent exudate.
- Pain, fever, anorexia, and depression may be present.
- Definition:

-
- Differential diagnoses:
- Mycetoma (should have grains in the draining exudate).
- Dermatophytic pseudomycetoma (mainly Persian cats).
- Atypical mycobacteriosis.
- Nodular panniculitis.
- Diagnosis:
- History (e.g. the cat has access to the outdoors, multi-cat household) and clinical signs.
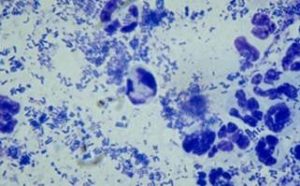
- Direct smear of exudate: rods, cocobacilli, cocci, degenerate neutrophils.
- Differential diagnoses:

-
- Treatment:
- Abscesses should be surgically drained and thoroughly flushed with saline or chlorhexidine solution. This treatment may suffice in some cases.
- Systemic antibiotics is required in many cases. Ideally, select the antibiotic based on culture and susceptibility test results. A “first choice drug” should be selected whenever possible. These include amoxicillin clavulanic acid, cefalexin, cefadroxil and clindamycin. Treatment has to be continued until resolution of clinical signs. Recheck to determine.
- Be sure to perform a culture and susceptibility test in resistant cases (Nocardia spp. and Actinomyces spp. organisms may be involved).
- If culture is negative, it is possible that L-form bacteria are the cause of the infection. L-form bacteria are partially cell wall-deficient. These bacteria cannot be cultured by routine techniques. Treat empirically with tetracyclines.
- If intact male, consider castration: effective in 80-90% of the cats as preventative.
- Be sure to also perform FIV and FeLV tests in resistant cases and all cats with outdoor access.
- Treatment:
Important Facts
- Bacterial folliculitis and deep pyoderma are less common in cats than in dogs.
- Abscess and cellulitis from fight wounds is one of the most common cat diseases handled in a small animal practice.
- They are caused by bacteria from the cat’s teeth and claws that lodge in the dermis and subcutaneous tissue during fights.
- Treatment involves surgical drainage and thorough flushing of the abscess and this may be the sole therapy in some cases.
- Systemic antibiotic is required in many cases.
- Select the antibiotic based on culture and susceptibility and choose a “first choice drug” whenever possible. These include amoxicillin clavulanic acid, cefalexin, cefadroxil and clindamycin.
- Continue systemic antibiotic therapy until the infection is resolved.
- Recheck the patient before discontinuing the antibiotic therapy.
References
Kennis RA, Wolf AM. Chronic bacterial skin infections in cats. Comp Cont Educ 1999; 21(12): 1108-1162.
Scott DW, Miller WH, Griffin CE: Small Animal Dermatology. 5th edn. Philadelphia: W.B. Saunders Co., 1995; 311.
Woolley KL et al. Reduced in vitro adherence of Staphylococcus species to feline corneocytes compared to canine and human corneocytes. Vet Dermatol 2007; 19:1-6.

