3.2 Feline Demodicosis
Learning Objectives
- Know that three Demodex mites can cause feline demodicosis.
- Know the different clinical and therapeutical aspects between these two forms of demodicosis.
- Learn the treatment options to manage feline demodicosis.
- Know the rule-of-thumb regarding treatment duration of feline demodicosis caused by the D. cati, unnamed mite species, and D. gatoi.
-
General Considerations
- Demodex cati: follicular mite similar to Demodex canis except that it is smaller and the ova are slim and oval, rather than spindle-shaped. Life cycle and mode of transmission not well understood.
- Cats can have localized or generalized demodicosis as in the dog.
- Demodex gatoi (surface mite): not a follicular mite but rather exists within the stratum corneum. It has a broad blunted abdomen instead of a slim elongated one. The life cycle and mode of transmission are unknown.
- Demodex sp. (unnamed species): this mite is smaller than D. cati and longer than D. gatoi. Very little is known about the biology of this mite.
- Cats can be infested with all three species of mites.
- A novel quantitative polymerase chain reaction assay (qPCR) found that the three feline Demodex species have distinct genotypes indicating that they are indeed three different species.
- Demodex cati: follicular mite similar to Demodex canis except that it is smaller and the ova are slim and oval, rather than spindle-shaped. Life cycle and mode of transmission not well understood.
-
Pathogenesis
- Demodex cati – It is usually associated with a systemic disease and an immunodeficiency state such as FIV infection, diabetes mellitus, toxoplasmosis, hyperadrenocorticism, squamous cell carcinoma in situ and other neoplastic conditions. Immunosuppressive therapy can also trigger demodicosis caused by D. cati. In some cats, no underlying cause can be identified.
- Demodex gatoi (surface mite) – This is a contagious mite. Affected cats are usually young and healthy but older cats and cats with signs of systemic illness should be evaluated for an underlying disease.
- Demodex sp. – Reports have indicated that the unnamed species of Demodex is more common in cats with concurrent illnesses and/or those recently recovered from a systemic disease, especially shelter cats.
-
History
- If owners complain of overgrooming, chewing or scratching in a young, otherwise healthy cat, or if you notice broken hairs at sites of alopecia or hypotrichosis be suspicious of surface demodicosis (D. gatoi). The history of more than one cat affected in the household should also increase the index of suspicion for the surface demodicosis because D. gatoi mites are contagious. Keep in mind that not all cats harboring the mites will have clinical signs.
- If owners complain of alopecia in a middle age to older cat with a comorbidity, be suspicious of follicular demodicosis (D. cati). Pruritus may be present but uncommonly. If it is present, another possibility to consider is the concurrent presence of D. gatoi or of an underlying allergic disease.
- If owners complain of alopecia associated or not with pruritus in a cat with concurrent disease or that has recovered from a systemic illness be suspicious of the unnamed Demodex mite.
-
Clinical Signs
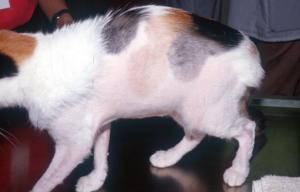
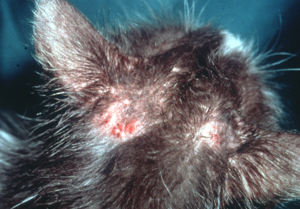
- Demodicosis caused by Demodex cati and Demodex sp.
- The disease can be localized or generalized.
- Combinations of alopecia, hypotrichosis, scaling, crusting, erythema, and hyperpigmentation can be present.
- Some cats will have a sparse hair coat and greasy skin.
- Some cases may be limited to the chin and perioral area and mimic acne.
- Ceruminous demodectic otitis externa may occur.
- Demodicosis caused by Demodex gatoi (surface demodicosis) – It has a more variable presentation.
- The disease is typically pruritic.
- It often presents as symmetric, self-inflicted, non-inflammatory alopecia and it should be a differential diagnosis for cats with this clinical presentation.
- It can mimic classical signs of allergy characterized by self-induced and inflammatory alopecia.
- Remember that cats can asymptomatically carry this mite and that it is contagious!
- Demodicosis caused by Demodex cati and Demodex sp.


-
Diagnosis
- History and clinical signs.
- The follicular mite (D. cati) is easy to find on multiple deep skin scrapings (like D. canis in dogs).
- The surface mite (D. gatoi) can be difficult to find on multiple superficial skin scrapings because cats remove the mites from the skin surface when grooming. Perform multiple and broad scraping of large skin areas. Scrape also areas that are not clinically affected and that the cat cannot groom, such as the upper neck.

-
- Fecal flotation to look for the surface mite (D. gatoi) if multiple skin scrapings are negative.
- At this time, it is not known if the Demodex sp. mite inhabits the hair follicle or the skin surface and how easily they are found on skin scrapings. The recommendation is to perform both a trichogram and multiple skin scrapings to increase the chance of finding the mites.
- Multiple negative skin scrapings and a negative fecal flotation do not rule out the demodicosis caused by the surface mite (D. gatoi). A treatment trial with lime sulfur dips or another parasiticidal shown to be efficacious should be performed if the index of suspicion is high. The recommendation when doing the trial with lime sulfur dips is as follows: (i) no significant response after the third or fourth lime sulfur dip, surface demodicosis is less likely, (ii) significant improvement noted after the third or fourth treatment, finish the trial and dip all cats in the household.
- Full blood work (including FeLV and FIV titers) should be performed for demodicosis developing in middle age to older cats or any cat with concurrent illness.
-
Treatment
- If only a focal area is affected the following can be tried before considering more aggressive treatment:
- 1% rotenone ointment (Goodwinol; Goodwinol Products Group)
- 2% lime sulfur dips
- Ceruminous otitis:
- Canex (Pittman-Moore, Inc., Washington Crossing, New Jersey) mixed with mineral oil (1:3).
- Tresaderm is effective in some cases.
- A 0.01% ivermectin suspension available for the treatment of Otodectes (Acarexx®; Boehringer Ingelheim) may be effective.
- Follicular demodicosis (D. cati), un surface demodicosis (D. gatoi):
- Follicular demodicosis (D. cati):
- Fluralaner (Bravecto®): It is only labeled in the USA to treat flea and tick infections; however, it has been shown to be efficacious in the treatment of feline demodicosis. Topical (labeled for cats) or oral (only labeled for dogs) formulations. Use the same dose recommended for flea and tick control. Only one treatment may be needed. The first negative skin scrapings can be achieved as soon as one month after treatment initiation. Good safety profile. Do not use in animals with a history of seizures.
- Doramectin administered subcutaneously, once weekly at a dosage of 600 µg/kg (0.6 mg/kg) has been shown to be efficacious for follicular demodicosis (D. cati). It is a GABA agonist and potential side effects include mydriasis, hypersalivation, lethargy, ataxia, seizure, coma and death.
- Oral ivermectin at 300 µg/kg (0.3 mg/kg) orally, given weekly to daily has been effective in few cases. Explain to the client that this protocol is not labeled to manage feline demodicosis and very few cases have been treated at this time to adequately assess efficacy. It is a GABA agonist and potential side effects include mydriasis, hypersalivation, lethargy, ataxia, seizure, coma and death.
- Considering its easy administration and good safety profile, the authors recommend using fluralaner as the treatment of choice for follicular demodicosis caused by D. cati.
- Treatment duration – rule of thumb – Independent of the drug used, continue treatment until two consecutive skin scrapings obtained 4 to 6 weeks apart are negative.
- Identify and treat an underlying disease if possible for cases of follicular demodicosis (D. cati).For long-term treatment success, it is important to identify and treat any underlying disease.
- Surface demodicosis (D. gatoi):
- Lime sulfur dips: Weekly 2% lime sulfur dips for 6 to 8 treatments. Improvement is typically seen after four dips. Apply the solution thoroughly, allow it to soak for at least 5 minutes and drip-dry. Resistant cases have been anecdotally reported.
- Cats should ideally wear a collar until the dip solution is completely dry to prevent excessive ingestion of the solution, which may cause oral ulcerations. However, a study using bi-weekly lime sulfur dips to manage feline dermatophytosis did not report any side effects after up to 15 lime sulfur applications and none of the cats wore a device to prevent ingestion of the solution.
- Lime sulfur can cause skin irritation when applied frequently and it can dry the skin and hair coat.
- Fluralaner (Bravecto®): The dog’s oral formulation was used extra-label in two cats with surface demodicosis at the dose of 26-34 mg/kg. After one month, no mites were found on skin scrapings or fecal flotation and the skin lesions had resolved. A spot-on fluralaner is currently approved for cats. It was anecdotally reported to be also effective in treating surface demodicosis.
- Ivermectin: It was reported to be effective in one case when given orally at 300 µg/kg (0.3 mg/kg) every 2 days for 10 weeks. Tell pet owners to monitor the cat closely for potential side effects (listed above under follicular demodicosis). Moreover, explain that this protocol is not labeled to manage feline demodicosis and efficacy has not been validated in large numbers of cases. It is most likely to work best for the feline follicular demodicosis (D. cati).
- Selamectin (Revolution®; Zoetis): It was reported to be effective in treating one cat with surface demodicosis (D. gatoi) when applied at 12 mg/kg every 30 days for 5 months. Efficacy needs to be validated in a larger number of cases.
- Advantage Multi® (Bayer HealthCare LLC; Whippany, NJ), (10% imidacloprid + 2.5% moxidectin): It was reported to be effective in treating surface demodicosis when applied weekly for 8 to 10 treatments. The authors did not find this treatment modality to be efficacious to treat feline surface demodicosis. In general, it has a good safety profile but application-site reaction and rarely lethargy, hypersalivation, depression, mydriasis and muscle tremors can occur. Efficacy needs to be validated in a larger number of cases.
- Considering its easy administration and good safety profile, the authors recommend using fluralaner as the treatment of choice for surface demodicosis caused by D. gatoi.
- Treatment duration – It varies according to the parasiticidal used and the recommended treatment protocol. Unfortunately, treatment duration cannot be based on negative skin scrapings as for the follicular mites because surface mites are not easily found on skin scrapings or fecal flotation. Clinical signs will dictate treatment duration.
- Feline demodicosis caused by the surface mite is contagious and all cats in the household should be treated even if clinical signs are not present because some cats can be asymptomatic carriers.
- Consider an underlying allergy in cats with surface demodicosis that continue to be pruritic after adequate treatment.
- Lime sulfur dips: Weekly 2% lime sulfur dips for 6 to 8 treatments. Improvement is typically seen after four dips. Apply the solution thoroughly, allow it to soak for at least 5 minutes and drip-dry. Resistant cases have been anecdotally reported.
- Unnamed Demodex sp.
- Ivermectin: Oral ivermectin at 0.3 mg/kg q 24h in conjunction with twice-weekly lime sulfur dips for 6 to 8 weeks has been effective. Ivermectin has shown to be effective as sole therapy when administered subcutaneously at 0.6 mg/kg q 24h for 4 weeks. Efficacy of these protocols needs to be validated in a larger number of cases.
- Isoxazolines: Treatment of this demodicosis using fluralaner or another isoxazoline has not been reported, to our knowledge. However, it is likely to be effective and should be tried because of its easy administration and good safety profile.
- The authors recommend treating at least until two negative skin scrapings are obtained at about 4-week intervals.
- Follicular demodicosis (D. cati):
- If only a focal area is affected the following can be tried before considering more aggressive treatment:
-
Client Education
- The diagnosis of surface demodicosis can be challenging because mites are difficult to find on multiple skin scrapings or fecal flotation. In addition, other pruritic diseases can present with signs similar to surface demodicosiss.
- Surface demodicosis is contagious and all cats in the household should be treated.
- Mention to pet owners that the current treatment modalities for feline demodicosis have not been validated in a large number of cases.
- The prognosis is guarded for middle age to older cats with follicular demodicosis because this disease is often associated with an underlying disorder that is not curable.
- At this time very little information has been reported regarding the demodicosis caused by the unnamed mite (Demodex sp.), which makes it difficult to provide accurate information on diagnosis, treatment and prognosis.
Important Facts
- Surface demodicosis caused by D. gatoi can be pruritic and is contagious.
- Self-induced non-inflammatory alopecia is a common clinical presentation of surface demodicosis.
- Alopecia, scaling and erythema are common signs of feline follicular demodicosis caused by D. cati.
- Demodicosis caused by D. cati is usually associated with an underlying disease.
- Demodicois caused by the unnamed mite has been typically reported in cats with concurrent illness or that have recovered from a systemic illness.
- Treat until two consecutive negative skin scrapings at about 4-week intervals in cases of follicular demodicosis (D. cati) and the unnamed Demodex sp..
- Treat according to the recommended protocols for cases of surface demodicosis (D. gatoi) and rely on clinical signs to determine duration of therapy because mites are difficult to find on skin scrapings.
References
Duangkaew L and Hoffman H. Efficacy of oral fluralaner for the treatment of Demodex gatoi in two shelter cats. Vet Dermatol 2018; 29:262.
Matricoti I and Maina E. The use of oral fluralaner for the treatment of feline generalized demodicosis: a case report. J Small Anim Pract 2017; doi: 10.1111/jsap.12682. [Epub ahead of print].
Miller WH, Griffin CE, Campbell KL. Small Animal Dermatology, 7th ed. St. Louis, MO: Elsevier, 2013; 284-342.
Moriello KA, Newbury S, Steinberg H. Five observations of a third morphologically distinct feline Demodex mite. Vet Dermatol 2013; 24:460-463.
Mueller RS, Rosenkrantz W, Bensignor E et al. Diagnosis and treatment of demodicosis in dogs and cats – Clinical consensus guidelines of the World Association for Veterinary Dermatology. Vet Dermatol 2020; 31: 4-e2. DOI: 10.1111/vde.12806
Saari SA, Juuti KH, Palojarvi JH et al. Demodex gatoi-associated contagious pruritic dermatosis in cats – a report from six households in Finland. Acta Veterinaria Scandinavica 2009; 51: 40-47.
Short J and Gram D. Successful treatment of Demodex gatoi with 10% imidacloprid/1% moxidectin. J Am Anim Hosp Assoc 2016; 52:68-71.
Silbermayr K, Horvath-Ungerboeck C, Eigner B et al. Phylogenetic relationships and new genetic tools for the detection and discrimination of the three feline Demodex mites. Parasitol Res 2015; 114(2):747-52.

