3.3 Demodicosis – Large Animals
Learning Objectives
- Know the clinical signs associated with bovine, caprine, swine, equine and ovine demodicosis. In most animal species listed here, the clinical signs are different from the ones in dogs and cats.
- Remember that demodicosis is not a contagious disease.
- Learn how to diagnose demodicosis in the animal species discussed in this chapter.
- Learn how to manage demodicosis in the animal species discussed in this chapter.
-
General Considerations
- Demodectic mange is a follicular dermatosis of cattle, goats, pigs and, rarely, sheep and horses.
- Demodectic mites are normal skin residents.
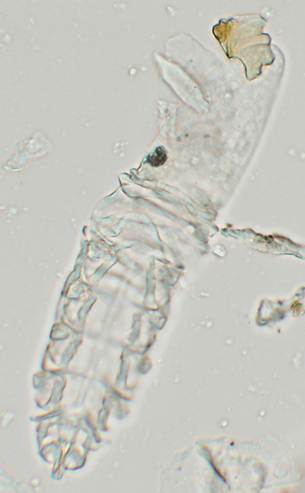
- The mites live in the hair follicle and sebaceous glands, are host-specific and complete their entire life cycle on the host. The life cycle is assumed to be completed in 20 to 35 days
- It appears that mites cannot survive very long off the host when exposed to most environmental conditions.
- Because Demodex mites are normal residents of the skin, it is likely that animals manifesting clinical disease are immunocompromised in some manner.
-
Bovine Demodicosis
- Cause:
- There are three currently known bovine Demodex (D.) mites: D. bovis, D. ghanensis and D. tauri. It is not known if D. ghanensis or D. tauri cause skin disease.
- Clinical Signs:
- Animals in poor condition are predisposed.
- Genetic possibly participates in disease development because in the USA Holsteins are commonly affected.
- The disease occurs in animals of all ages.
- Lesions are usually asymptomatic and present as follicular papules and nodules especially over the withers, neck, back, and flanks.
- Cause:

-
-
- Generalized skin involvement can occur.
- The overlying skin is usually normal in appearance.
- Occasionally, ulceration, fistula, abscess, and crust may be seen, especially if follicular rupture or secondary bacterial infection or both, has occurred.
- Demodicosis is seen more frequently in adult dairy cattle in late winter and spring.
- It is not contagious.
- Diagnosis:
- History and clinical signs.
- Deep skin scrapings of skin covering nodules may be unrewarding. There is a higher chance to find mites when scraping papules.
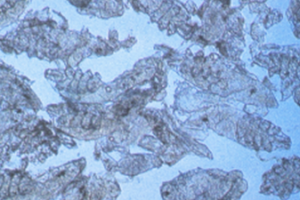
- If deep skin scraping are negative, incise the surface of papules and nodules. Evacuate the content manually, which is characterized by a thick, caseous and whitish material. Place the content in a glass slide and mixed it well with mineral oil to make a thin and uniform layer. Lower the microscope condenser to best visualize the mites, which are typically in large numbers.
- Skin biopsy is rarely needed to diagnose the disease.
- Treatment:
- 2% trichlorfon (Neguvon®; Bayer AG) applied as a total body dip every-other-day for three treatments can be curative. However, treatment is not usually attempted because the disease is often asymptomatic, may spontaneously regress, and has been refractory to most therapeutic agents and regimens.
- Make sure herd management is adequate and the affected animal is healthy otherwise.
- Severe infestations may result in significant economic loses through hide damage.
- Consider culling severely affected animals.
-
-
Caprine Demodicosis
- Cause:
- Demodex caprae
- Clinical Signs:
- Asymptomatic follicular papules and nodules on the face, neck, shoulders and sides.
- A thick keratin-sebaceous material can be expressed from the nodules. This material contains large numbers of mites.
- The overlying skin is typically unaffected.
- It is not contagious.
- Cause:


-
- Diagnosis:
- Same diagnostic plan as described for bovine demodicosis.
- Diagnosis:
-
- Treatment:
- Localized nodules can be incised, the content expressed manually, and the empty spaces infused with either Lugol’s iodine or rotenone in alcohol (1:3).
- Generalized lesions:
- Ronnel, a organophosphorus insecticide, in propylene glycol – 180 ml of 33% ronnel in 1000 ml of propylene glycol. Apply the solution to one third of the body once daily until cure is achieved. Clip the hair coat if necessary.
- Rotenone in alcohol (1:3) applied to one fourth of the body once daily until the whole body has been treated (i.e. 4 days). Treat until cure is achieved.
- Make sure herd management is adequate and the affected animal is, otherwise, in good health.
- Treatment:
-
Swine Demodicosis
- Cause:
- Demodex phylloides
- Clinical Signs:
- Swine demodicosis is usually asymptomatic and characterized by skin colored or erythematous follicular papules, pustules and nodules especially on snout, eyelids, ventral neck, ventral thorax, ventral abdomen, and medial thighs.
- Cause:

-
-
-
- Secondary staphylococcal pyoderma may occur.
- Diagnosis:
- Same diagnostic plan previously described for bovine demodicosis.
- Because mites are part of the skin fauna, it is not sufficient to give a diagnosis if one or two are found in samples. Demonstration of an actively growing mite population (i.e. large number of immature stages) and characteristic lesions justify the diagnosis of demodicosis.
- Treatment:
- No treatment is required in most cases because the disease is often asymptomatic.
- 2% trichlorfon has been reported to be curative and can be tried in some cases. Use the protocol described for cattle.
- Severely affected pigs should be culled from the herd.
- Make sure herd management is adequate and the affected animal is, otherwise, in good health.
-
-
-
Ovine Demodicosis
- Cause:
- Demodex ovis
- Clinical Signs:
- Uncommon to rare in occurrence.
- Clinical signs include asymptomatic alopecia, erythema and scaling of the face, neck, shoulders, and back. Crusts, pustules, and abscesses may also be seen.
- Pinnae, limbs, and coronets are typically affected.
- Diagnosis:
- Multiple deep skin scrapings. Mites are easy to find.
- Treatment:
- No treatment is required in most cases.
- 2% trichlorfon as described for cattle has been reported to be curative.
- Make sure herd management is adequate and the affected animal is, otherwise, in good health.
- Cause:
-
Equine Demodicosis
- Cause:
- There are two Demodex species found in horses: Demodex equi and Demodex caballi. Demodex caballi appears to be limited to the eyelids and muzzle, while Demodex equi resides on the body.
- Cause:
-
- Clinical Signs:
- Asymptomatic alopecia and scaling, especially on the face, neck, shoulders, and forelimbs.
- Follicular papules and pustules may be seen.
- Diagnosis:
- Multiple deep skin scrapings. Mites are easy to find.
- Treatment:
- The disease seems to be refractory to most treatment regimens used for demodicosis.
- Search for an underlying cause including chronic use of immunosuppressive drugs such as glucocorticoids.
- Spontaneous regression is possible if an underlying cause is identified and successfully controlled and immunosuppressive drugs are discontinued.
- Make sure the general care of the horse is adequate (i.e. proper feeding and exercise, vaccination, parasite control, dental care etc.).
- Do not use amitraz in horses.
- Side effects include somnolence, depression, ataxia, muscle weakness, and large intestine impaction.
- Clinical Signs:
Important Facts
- Demodicosis is a rare disease in large animals.
- In cattle, goats and pigs, asymptomatic follicular papules and nodules are the characteristic clinical signs.
- In horses and sheep, nodules are not seen and alopecia, scaling and erythema are the main clinical signs. Follicular papules and/or pustules are occasionally present.
- If deep skin scrapings are negative, incise any nodules present and examine under the microscope the thick, caseous content. Mites are usually in large numbers.
- Treatment is not typically attempted. Identify and control or cure underlying diseases and discontinue immunosuppressive drugs if possible.
- Make sure the general care of affected animals is adequate (i.e. proper feeding, vaccination, parasite control, dental care etc.).
- Cull severely affected animals.
References
Greves JH, Davies P. External parasites. In: Diseases of swine. 10th edn. Wiley, Ames 2012; 885-894.
Kral F, Schwartzman RM. Veterinary and comparative dermatology. Philadelphia: J.B. Lippincott Co., 1964.
Nutting WB. Hair follicle mites (Demodex spp.) of medical and veterinary concern. Cornell Vet 1976; 66: 214-31.
Scott DW. Parasitic Diseases. In: Large Animal Dermatology. Philadelphia, PA: W.B. Saunders, 1988; 226-230.
Scott DW. Color atlas of farm animal dermatology. Ames, IA: Blackwell Publishing, 2007; 21–33 cattle; 115–123 goats; 159–166 sheep; 209–213 pigs.
Scott DW, Miller WH Jr. Equine dermatology. 2nd edn. Philadelphia: W.B. Saunders, 2011; 221-222.

