3.1 Canine Demodicosis
Learning Objectives
- Identify the stages of the life cycle of the Demodex mite.
- Know the clinical characteristics of the localized and generalized juvenile-onset and adult-onset forms of demodicosis (age of onset, distribution of lesions, clinical signs, genetic predisposition, prognosis).
- Learn the predisposing factors of adult-onset demodicosis.
- Learn the predisposing factor of juvenile-onset generalized demodicosis.
- Learn how to treat localized and generalized demodicosis (discuss all treatment options).
- Learn the potential side effects associated with the drugs used to manage canine demodicosis.
- Understand why corticosteroids and other immunosuppressive drugs are contraindicated in dogs with demodicosis.
- Know the treatment duration rule-of-thumb and make sure to apply it when treating a dog with demodicosis.
- Know the rule to declare remission and cure when treating a dog with demodicosis.
-
General Considerations
- Currently, there are two different species of demodex mites that can cause demodicosis in dogs: Demodex canis and Demodex injai. The clinical signs associated with disease caused by each of these parasites are different and because demodicosis caused by Demodex canis is more frequently seen, more information will be provided on this disease sub-type. Demodex canis is a normal inhabitant of canine hair follicles and, less commonly, the sebaceous glands (see below more details about this form of mange).
- Demodex injai also inhabits the hair follicles and especially the sebaceous glands. It is not known, however, if these mites are part of the normal skin fauna but the general belief is that they are. Demodex injai mites are longer than D. canis mites and the typical clinical presentation is excessive oil along the dorsum with no or mild hypotrichosis. The face may also be affected. The associated skin is often erythematous. It has been reported more frequently in adult dogs of smaller breeds and allergic dermatitis appears to be a common coexisting disease. Pruritus can be mild to intense and may reflect a coexistent allergic condition. Mite numbers are typically low thus; broad, deep skin scrapings of multiple sites should be performed to increase the likelihood of finding the mites.
- Canine demodicosis is an inflammatory parasitic disease. The disease caused by D. canis is associated with an immunologic dysfunction that allows large numbers of mites to proliferate in the hair follicles, which can eventually rupture leading to draining tracts (furunculosis). Secondary bacterial infection is also an aggravating factor.
- Demodex canis mites are transmitted from the mother to the neonate during the first 2 to 3 days of nursing and become part of the skin microbiota. The biology of the mange caused by the long-bodied D. injai mite is not well-understood.
- Breed predilection suggests that genetic plays a role in the pathomechanism of canine demodicosis.
- The entire life cycle of 20 to 35 days is completed on the host.
- Four stages of the life cycle may be demonstrated in skin scrapings: fusiform eggs, six-legged larvae, eight-legged nymphs and eight-legged adults.
- Demodicosis caused by these mites is not considered a contagious disease.
- Avoid using immunosuppressive drugs in patients with demodicosis.
-
Pathogenesis of demodicosis caused by D. canis
- The pathogenesis of the disease state associated with the proliferation of demodex mites is not completely understood.
- Most animals harbor very low numbers of mites inside their hair follicles and sebaceous glands. A study was able, for the first time, to demonstrate that healthy dogs indeed harbor Demodex mites in low numbers in haired skin. The authors used a real-time PCR method to amplify Demodex DNA from plucked hairs.
- When a benign resident organism becomes associated with disease, one must question the integrity of the immune system.
- Antilymphocyte serum given to very young puppies will cause them to develop generalized demodicosis.
- In vitro lymphocyte blastogenesis studies showed an abnormal lymphocyte response in dogs with generalized demodicosis suggesting that a faulty immune response was responsible for the mite proliferation. However, other studies showed that the suppressed blastogenesis response was caused by a humoral immunosuppressive factor likely produced by the mites. This factor and not a pre-existent cause suppressed the skin immune response and allowed the mite proliferation to continue unchecked.
- Other studies suggested that the suppressed lymphocyte blastogenesis response was a consequence of secondary bacterial pyoderma, often present in dogs with demodicosis.
- It is possible that both, the mites and the pyoderma, contribute to an abnormal cutaneous immune response that favors mite multiplication.
- An appealing theory is the presence of a hereditary Demodex canis-specific T cell defect of varying severity.
- The tendency to develop juvenile-onset generalized demodicosis is familial. Some bitches and sires will produce litter after litter of affected puppies and the predominance of the disease in certain breeds is also supportive of the contribution of genetics in disease development.
-
Classification and clinical signs of demodicosis caused by D. canis
- Classification:
- Juvenile-onset
- Localized
- Juvenile-onset localized demodicosis:
- The localized disease is characterized by few lesions.
- It typically affects dogs younger than 1 year of age.
- Most cases resolve spontaneously within 6 to 8 weeks.
- About 10% will become generalized.
- Pruritus can occur if secondary pyoderma develops.
- Main differentials include dermatophytosis and superficial pyoderma.
- Juvenile-onset localized demodicosis:
- Localized
- Juvenile-onset
- Classification:


-
-
-
- Generalized
- Juvenile–onset generalized demodicosis:
- Indications of generalized demodicosis:
- Many lesions distributed throughout the body.
- Indications of generalized demodicosis:
- Juvenile–onset generalized demodicosis:
- Generalized
-
-


-
-
-
-
-
-
- Involvement of an entire body region (e.g. facial area).
-
-
-
-
-

-
-
-
-
-
-
- Two or more paws affected.
-
-
-
-
-


-
-
-
-
-
-
-
- It usually starts as localized lesions that progress to become generalized.
- Dogs between 3 and 18 months of age are more often affected.
- Rare cases recover spontaneously.
- Affected dogs appear to have a genetic predisposition. Neuter these animals!
-
-
- Adult-onset
- Dogs that first develop the disease at 4 years of age or older are considered to have adult-onset demodicosis.
- It is typically associated with an underlying systemic disease such as Cushing’s (especially iatrogenic), hypothyroidism and malignant neoplasia. Long-term treatment with immunosuppressive drugs can also cause adult-onset demodicosis.
- Similar to the juvenile form, the disease can be localized or generalized.
- In a subset of cases, no underlying disease can be identified at the time the demodicosis is diagnosed. These cases should be monitored closely because systemic illness may become obvious weeks to months into treatment of the demodicosis.
-
-
-
-
-
- Clinical signs of demodicosis caused by D. canis:
- Localized:
- Lesions are usually mild and consist of one to several scattered patches of alopecia associated with scaling, erythema and/or hyperpigmentation.
- Areas especially affected are the periocular region, commissures of the mouth, head and forelegs. Patches may also be seen on the trunk.
- Generalized:
- Signs are extremely variable!
- Lesions include generalized patchy to diffuse alopecia associated with erythema, scaling, folliculitis (papules and pustules), furunculosis (draining tracts), seborrhea, and hyperpigmentation.
- Look closely for comedones (“blackheads”). These are usually good areas to scrape for mites!
- Localized:
- Clinical signs of demodicosis caused by D. canis:

-
-
-
- It is usually non-pruritic but it can become pruritic if secondary bacterial infection and seborrhea oleosa are present.
- Often, there is secondary superficial and/or deep pyoderma. Clinically, the pyoderma will present as papules, pustules, exudation from draining tracts, and/or crusts. Keep in mind that these lesions are also caused by the mites!
-
-

-
-
-
- Depending on the secondary pyoderma and disease severity, the dog may be systemically ill (fever, lethargy, poor appetite).
- Peripheral lymphadenopathy may occur and especially in the presence of furunculosis.
- Major differential diagnoses include superficial pyoderma and dermatophytosis for cases with well-demarcated alopecia, scaling and hyperpigmentation and deep pyoderma for cases with draining tracts.
- Every dog with pododermatitis should be scrapped for demodicosis.
-
-
-
Diagnosis
- History and clinical signs are important part of the diagnosis equation.
- Multiple deep skin scrapings performed until capillary bleeding occurs.
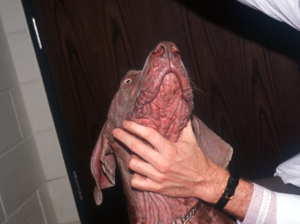
- Before scraping, fold and squeeze the affected skin to extrude mites from the hair follicles canals.
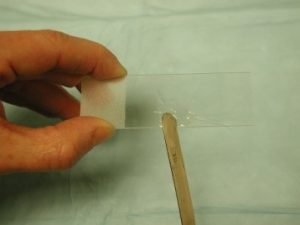
- Before scraping, wet with mineral oil the instrument or the skin area you will scrape. These will allow the samples to adhere to the instrument you are using to scrape the skin.




-
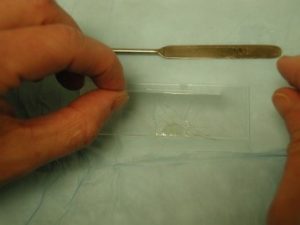
- Place the scraped material in a few drops of mineral oil on a microscope slide and apply a coverslip.
-
- Examine the sample under the 10x objective and make sure to lower the microscope condenser to increase contrast and allow the mites to be seen more readily.
- Demodex canis mites are easy to find on properly performed skin scrapings! However, D. injai can be difficult to find likely because they are present in smaller numbers and can lodge primarily in sebaceous glands. Therefore, to increase your chances to find mites perform multiple scrapings covering a broad area. Moreover, fold and squeeze the affected skin before scraping. This will help bring mites to the skin surface and upper portion of the follicle canal.
- Avoid scraping areas of fibrosis because they are difficult to scrape and often yield no mites.
- In general and if properly performed, negative skin scrapings can rule out demodicosis caused by D. canis. However, the excessive mucopolysaccharide present in the skin of shar-pei dogs may impede the extrusion of mites from hair follicles resulting in false negative results.
- Trichoscopy may also reveal mites in severe cases of demodicosis caused by D. canis. Various hairs are plucked from affected areas, placed in mineral oil on a glass slide and covered with a coverslip before microscopic evaluation. This test is not as sensitive as skin scrapings but is more sensitive than the acetate tape impression with squeezing test (see below). It should be used in areas that are difficult to scrape such as, the face and paws. If no mites are found, perform skin scrapings before ruling out demodicosis.
- Acetate tape impression with squeezing of affected skin has been reported as a diagnostic test for demodicosis. The method involves the following: (i) place a transparent acetate tape on affected areas; (ii) fold and squeeze the skin where the tape was placed; (iii) remove the tape; (iv) place the tape directly on a glass slide; (v) exam under microscope. This test should be used in areas that are difficult to scrape such as the face and paws but should not replace the skin scrape. If no mites are found, perform skin scrapings before ruling out demodicosis. The authors prefer the trichoscopy test for sampling the face and paws than the acetate tape impression with squeezing.
- Mites can also be found on cytology of exudate collected from draining tract lesions.
- Interpretations of skin scrapings:
- Many immature and adult mites: diagnostic.
- One to two adult mites: scrape again as rarely the presence of few demodex mites on scrapings is an insignificant finding.
- No mites: scrape again or reconsider the diagnosis.

-
- Histopathology:
- Skin biopsy is usually not necessary for the diagnosis of demodicosis. However, in Chinese shar-pei dogs biopsies may be needed if multiple and properly performed skin scrapings yield no mites.
- Histopathology:
-
Treatment: Do not use immunosuppressive drugs (systemic or topical)!
- Localized:
- No treatment may be needed because the large majority of cases resolve spontaneously.
- Topical 1% rotenone Goodwinol ointment can be applied daily to lesions.
- Benzoyl peroxide shampoo or gels can be used for their follicular flushing action and to prevent secondary bacterial infections.
- Improve nutrition, treat intestinal parasites and remove other stress factors.
- Amitraz or systemic parasiticidal therapy are not rational treatments for localized demodicosis when 90% will spontaneously resolve. Do not risk the development of resistant mites.
- Generalized:
- Correct any nutritional, parasitic, or other concurrent problems.
- Dogs with adult-onset demodicosis should receive a full diagnostic workup to look for underlying diseases. A CBC, serum chemistry profile, urinalysis, urine culture, HWT and fecal parasite exam, along with thyroid and Cushing’s evaluation should be performed if suspecting of these disorders. Ultrasonography and radiographic or advanced imaging should also be performed if indicated.
- Secondary poderma:
- A study showed that secondary bacterial skin infections often resolve after the treatment of demodicosis. Therefore, systemic antibiotic therapy may not be required for most cases. However, if the dog has generalized demodicosis associated with severe secondary deep pyoderma, systemic antibiotic may be required. If antibiotic is required, the selection should be based on bacterial culture and sensitivity. Because lesions of superficial and deep pyoderma mirror lesions of demodicosis you cannot use the rule of thumb of treating pyoderma until complete resolution of clinical signs. Therefore, in cases of demodicosis associated with pyoderma we recommend performing cytology of lesions at each recheck appointment to evaluate for the presence bacterial infection. Ideally, a culture and sensitivity should be performed before considering discontinuation of antibiotic therapy.
- The hair coat should be clipped, especially long- and medium-haired dogs, if you prescribe topical therapy such as amitraz. You want the solution to effectively contact the skin.
- Bathe the dog with an antibacterial, keratolytic and follicular flushing shampoo (e.g. benzoyl peroxide) to open the hair follicles and remove the crusts before applying the amitraz solution.
- Rule-of-thumb for treatment with all parasiticidals -Treat for 30 days after two consecutive negative skin scrapings are obtained at 4 or 8 weeks intervals (i.e.: first negative scrapings—– treat for 4 to 8 weeks—-second negative scrapings ——- treat for 30 more days and then stop therapy).
- About 50% to 80% of the cases will be in remission after 3 months of therapy. However, it may take much longer before remission can be achieved.
- Continue to monitor the dog with skin scrapings throughout the following year before declaring the dog cured.
- Dogs with a non-curable underlying disease may have chronic demodicosis and will need therapy for life.
- Female dogs should be spayed when the disease is under control because the estrus cycle may cause the disease to relapse.
- Dogs with juvenile-onset generalized demodicosis should be neutered.
- Amitraz (Mitaban®):
- Currently, the only FDA approved product to treat canine demodicosis in the US is amitraz. It is licensed for use at the concentration of 250 ppm (i.e. one vial is diluted in two gallons of lukewarm water) applied every 14 days.
- For greater efficacy, weekly dips may be needed. Resistant cases may need a double strength concentration of 500 ppm weekly.
- Small dogs should receive one-half strength of amitraz solution at the first dipping (Chihuahuas are very sensitive).
- Pour and sponge the amitraz solution throughout the skin until the patient is completely wet. Let the solution drip dry or blow dry the dog’s coat.
- Do not let the dog get wet in between dips.
- Prepare the solution immediately before using and throw away any leftover. Amitraz is not very stable after mixed with water.
- Monitor the pet closely for side effects. Side effects include sedation, pruritus, hypothermia, ataxia, and disorientation for 24 to 36 hours, especially after the first dip. Do not stress the animal for 24 hours following application. Amitraz can also cause hyperglycemia (at two times the recommended concentration) and should not be used in diabetic dogs.
- Do not apply to sedated or anesthetized dogs.
- Antihistamines such as hydroxyzine or doxepin should NOT be used as they can potentiate the effect of monoamine oxidase inhibitors such as amitraz. For pruritus, diphenhydramine can be tried (usually ineffective).
- Antidote for amitraz is yohimbine 0.1 mg/kg IV.
- Commonly used off label (USA) options:
- Daily amitraz (Taktic® 5%; MSD Animal Health) – dilute 10 mL of the 5% solution into one liter of water.
- daily ½ body applications.
- 79% cure rate.
- Note: This product is not Mitaban®. Taktic is amitraz in mineral oil; Mitaban® is amitraz in xylol.
- Continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4 to 8- week intervals (rule-of-thumb).
- Continue to monitor dog with skin scrapings over the following year before declaring a cure.
- Daily Ivermectin (Ivomec®; Merial):
- Ivermectin is a macrocyclic lactone. It opens glutamate sensitive chloride channels in neurons and myocytes of invertebrates resulting in hyperpolarization of these cells and and inhibition of signal transmission.
- Dosages range from 300 to 600 µg/kg q 24h (0.3 to 0.6 mg/kg q 24h) given orally. This dose is much higher than a regular heartworm prevention dose. It is wise to start low and increase the dosage daily by increments of 100 µg/kg (0.1 mg/kg) before achieving 600 µg/kg (0.6 mg/kg). This is a safe protocol to identify the dogs that cannot tolerate the drug.
- Use the cattle or pig 1% (10 mg/ml or 10,000 µg/ml) injectable ivermectin.
- Not FDA approved for the treatment of canine demodicosis.
- Continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4- to 8- week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- DO NOT USE: collies, Shetland sheepdog or its crosses; Australian shepherd; white Swiss shepherd, longhaired whippet, silken windhound, McNab, and Border collie. Breeds that the allele for the mutated ABCB1-1 gene (former MDR1 gene) has been detected but not homozygote for the mutation include the old English sheepdogs, Waller, and English shepherd. Ideally avermectins should not be used in these breeds. Currently, there is a genetic test available at the Washington State University (https://vcpl.vetmed.wsu.edu/) that can identify the ABCB 1 gene mutation associated with avermectin toxicity. This gene encodes for P-glycoprotein, which is responsible for pumping-out substances that cross the blood-brain barrier.
- It is also important to keep in mind that breeds considered non-sensitive to macrocyclic lactone toxicity could also develop neurotoxicity when treated with this group of drugs at the dose range and frequency recommended to manage demodicosis. In a study, dogs receiving ivermectin, milbemycin or moxidectin showed neurologic signs 4 days to 10 weeks after initiation of therapy. None of these dogs had mutation of the ABCB1-1 gene indicating the involvement of a different mechanism in the development of toxicity.
- Side effects are neurological and include mydriasis (typically the first side effect), ataxia, tremors, seizures, coma, and death.
- Daily milbemycin oxime (Interceptor®: Elanco):
- Milbemycin oxime is a macrocyclic lactone. It opens glutamate sensitive chloride channels in neurons and myocytes of invertebrates resulting in hyperpolarisation of these cells and and inhibition of signal transmission.
- Dosages range from 1.0 to 2.0 mg/kg q 24h (start low and increase dose if no or poor response after 30 days of therapy). Do not use higher doses to prevent side effects.
- Recheck every 4 to 6 weeks.
- Continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4- to 8- week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- Reported success rates: 60% to 100% but relapses were high (20%-40%). Our experience indicates that relapses occur in cases that are not treated long enough and/or not followed-up appropriately.
- Side effects are very rare in non-macrocyclic lactone sensitive breeds. However, it is wise to perform an ABCB1-1 (formerly MDR-1) mutation test in sensitive breeds since a study showed that dogs with a homozygous mutation for the gene developed neurologic signs at a dosage of 1.5 mg/kg q 24h. Remember that the ABCB1-1 gene encodes for P-glycoprotein.
- It is also important to keep in mind that breeds considered non-sensitive to macrocyclic lactone toxicity can also develop neurotoxicity when treated with this group of drugs at the dose range and frequency recommended to manage demodicosis. In a study, dogs receiving ivermectin, milbemycin or moxidectin showed neurologic signs 4 days to 10 weeks after initiation of therapy. None of these dogs had mutation of the ABCB1-1 gene indicating the involvement of a different mechanism in the development of toxicity.
- Imidacloprid 10% + moxidectin 2.5% (Advantage Multi® topical solution; Bayer HealthCare LLC; Whippany, NJ):
- Studies have shown its efficacy in treating mild cases of generalized demodicosis. This may be an alternative for the treatment of breeds sensitive to avermectins.
- Recommended treatment protocol: weekly to bi-weekly applications at the recommended dose for heartworm prevention or flea control. Studies have indicated that weekly applications result in better results than bi-weekly and dermatologists currently recommend weekly applications.
- Continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4 to 8 week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- It is not approved to treat demodicosis.
- Doramectin (macrocyclic lactone):
- It is an avermectin formulated as a 1% oil solution.
- Its plasma half-life is nearly twice that of ivermectin allowing less frequent administrations.
- Dose: 600 µg/kg subcutaneously or orally once weekly. It is wise to increase the dosage daily by increments of 100 µg/kg (0.1 mg/kg q 24h) before achieving the 600 µg/kg (0.6 mg/kg) dose. This is a safe protocol to identify the dogs that cannot tolerate the drug. The oral administration is more convenient than the subcutaneous. However, a study done in dogs (see reference below) showed a lower plasma concentration and a smaller area under concentration versus time curve for oral doramectin as compared to oral ivermectin.
- Continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4 to 8 weeks intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- DO NOT USE: collies, Shetland sheepdogs, or their crosses; Australian shepherds; white Swiss shepherds, longhaired whippet, silken windhound, McNab, and Border collie. Breeds that the allele for the mutated ABCB1-1 gene (former MDR1 gene) has been detected but not homozygote for the mutation include the old English sheepdogs, Waller, and English shepherd. Ideally avermectins should not be used in these breeds. Currently, there is a genetic test available at the Washington State University (https://vcpl.vetmed.wsu.edu/) that can identify the ABCB 1 gene mutation associated with avermectin toxicity. This gene encodes for P-glycoprotein, which is responsible for pumping-out substances that cross the blood-brain barrier.
- Side effects are neurological and include mydriasis (typically the first side effect), ataxia, tremors, seizures, coma, and death.
- Isoxazolines: They have been approved to treat demodicosis and other parasitic diseases in some countries.
- Fluralaner (Bravecto™ Chews and Spot-on, Merck Animal Health; Summit, NJ, USA):
- Fluralaner belongs to the isoxazoline class of insecticide and acaricide. The mode of action is the antagonism of the ligand-gated chloride channels (gamma-aminobutyric acid (GABA)-receptor and glutamate-receptor). Bravecto™ is marketed to provide 12 weeks of flea and tick control. It is labeled for dogs 6 months of age and older and should be given with food. It is currently licensed in the US to kill and prevent flea and tick infestations.
- The dose protocol to treat demodicosis is the same recommended to control flea and tick infestations.
- A spot-on product is also available and one tube has the same fluralaner concentration that one chew tablet has, so the dose is equivalent.
- A study showed that a single oral administration of Bravecto™ chewable tablets resulted in 100% reduction in mite numbers 56 and 84 days after treatment of dogs with generalized demodicosis. Similar efficacy was noted with the topically administered fluralaner.
- Continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4- to 8- week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- The most commonly reported side effect is vomiting.
- Isoxazolines have been reported to induce neurologic signs (e.g. tremors, ataxia, seizures) and should be used with caution especially in dogs with a history of seizures.
- Sarolaner (Simparica™ , Zoetis; Kalamazoo, MI, USA:
- Sarolaner belongs to the isoxazoline class of insecticide and acaricide. The mode of action of sarolaner is the same as fluralaner and involves the antagonism of the ligand-gated chloride channels (gamma-aminobutyric acid (GABA)-receptor and glutamate-receptor). The ultimate result is uncontrolled neuromuscular activity leading to the death of insects and acarines. It is currently licensed to kill and prevent flea and tick infestations.
- Studies have shown the efficacy of sarolaner to treat generalized canine demodicosis. The treatment protocol is the same recommended for flea and tick treatment/control. One chewable tablet calculated according to the pet’s body weight is given every 4 weeks. The tablet can be given with or without food.
- It is important to continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4- to 8-week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- Isoxazolines have been reported to induce neurologic signs (e.g. tremors, ataxia, seizures) and should be used with caution especially in dogs with a history of seizures.
- Afoxolaner (NexGard®, Merial; Duluth, GA, USA):
- Afoxolaner belongs to the isoxazoline class of insecticide and acaricide. The mode of action of afoxolaner is the same as fluralaner and involves the antagonism of the ligand-gated chloride channels (gamma-aminobutyric acid (GABA)-receptor and glutamate-receptor). The ultimate result is uncontrolled neuromuscular activity leading to the death of insects and acarines. It is currently licensed to kill and prevent flea and tick infestations.
- Studies have shown the efficacy of afoxolaner to treat generalized canine demodicosis. The treatment protocol is the same recommended for flea and tick treatment/control. One chewable tablet calculated according to the pet’s body weight is given every 4 weeks. The tablet can be given with or without food.
- In Europe, there is a formulation called NexGard Spectra® that contains milbemycin oxime in addition of afoxolanar. A study has shown its efficacy in treating generalized demodicosis in dogs (referenced below). In the US, NexGard Plus® contains milbemycin oxime and pyrantel in addition to afoxolaner. At this time, there are no studies investigating its efficacy in treating canine demodicosis.
- It is important to continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4- to 8- week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- Isoxazolines have been reported to induce neurologic signs (e.g. tremors, ataxia, seizures) and should be used with caution especially in dogs with a history of seizures.
- Lotilaner (Credelio®, Elanco; Greenfield, IN, USA):
- Lotilaner belongs to the isoxazoline class of insecticide and acaricide. As for the other isoxazolines its mechanism of action involves the antagonism of the ligand-gated chloride channels (gamma-aminobutyric acid (GABA)-receptor and glutamate-receptor). The ultimate result is uncontrolled neuromuscular activity leading to the death of insects and acarines. It is currently licensed to kill and prevent flea and tick infestations.
- Studies have shown the efficacy of lotilaner to treat generalized canine demodicosis. The treatment protocol is the same recommended for flea and tick treatment/control. One chewable tablet calculated according to the pet’s body weight is given every 4 weeks. The tablet can be given with or without food.
- It is important to continue treatment for 30 days after two consecutive negative skin scrapings are obtained at 4- to 8-week intervals (rule-of-thumb).
- Continue to monitor the dog with skin scrapings over the following year before declaring a cure.
- Isoxazolines have been reported to induce neurologic signs (e.g. tremors, ataxia, seizures) and should be used with caution especially in dogs with a history of seizures.
- Fluralaner (Bravecto™ Chews and Spot-on, Merck Animal Health; Summit, NJ, USA):
- Daily amitraz (Taktic® 5%; MSD Animal Health) – dilute 10 mL of the 5% solution into one liter of water.
- Localized:
-
Client Education
- Client education is very important in assuring a successful outcome.
- Management of demodicosis requires owners’ participation and commitment and they need to understand that.
- Focus the education on the form of demodicosis the pet has because recommendations differ to some extent.
- Remember to tell owners that the predisposition to develop juvenile-onset generalized demodicosis is inherited, so affected pets should not be bred.
- Discuss prognosis, which will vary according to the disease form.
- Set expectations regarding the various visits often required to treat the juvenile-onset generalized demodicosis and the adult-onset disease.
- Tell clients what will be done at each recheck visit and the associated costs. This is important to assure compliance.
Important Facts
- Disease forms: Juvenile-onset localized and generalized; adult-onset localized and generalized.
- Most cases of juvenile-onset localized demodicosis spontaneously resolve within 6 to 8 weeks.
- It is not currently known how many dogs with generalized demodicosis will have their disease resolve spontaneously. Nevertheless, treatment is typically instituted in this form of the disease, which is often severe.
- It is believed that dogs with juvenile-onset generalized demodicosis have a genetic predisposition. Therefore, affected dogs should not be bred.
- Look for an underlying systemic disease or a factor such as neoplasia, Cushing’s disease, hypothyroidism and use of immunosuppressive drugs in dogs that develop demodicosis at an adult age.
- Treat demodicosis for 30 days past two consecutive negative skin scrapings obtained at 4- to 8-week intervals.
- Continue to monitor the animal with skin scrapings over the following year before declaring cure!
- The adult-onset form has a guarded prognosis. The juvenile-onset generalized form has a fair to good prognosis and the juvenile-onset localized form has an excellent prognosis.
- If negative skin scrapings are never obtained during treatment, find an appropriate maintenance therapy.
References
Barbet JL, Snook T, Gay JM, et al. ABCB1-1 Delta (MDR1-1 Delta) genotype is associated with adverse reactions in dogs treated with milbemycin oxime for generalized demodicosis. Vet Dermatol 2009; 20(2): 111-114.
Beugnet F, Halos L, Larsen D et al. Efficacy of oral afoxolaner for the treatment of canine generalized demodicosis. Parasite 2016; 23:14. DOI: 10.1051/parasite/2016014.
Bissonnette S, Paradis M, Daneau I, et al. The ABCB1-1 Delta mutation is not responsible for subchronic neurotoxicity seen in dogs of non-collie breeds following macrocyclic lactone treatment for generalized demodicosis. Vet Dermatol 2009; 20 (1): 60-66.
Fourie JJ, Liebenberg, JE, Horak IG et al. Efficacy of orally administered fluralaner (Bravecto™) or topically applied imidacloprid/moxidectin (Advocate®) against generalized demodicosis in dogs. Parasites & Vectors 2015; 8: 187-193.
Gokbulut C, Boyacioglu M, Karademir U. Plasma pharmacokinetics and faecal excretion of ivermectin and doramectin following oral administration in donkeys. Res Vet Sci 2005; 79(3): 233-38.
Lebon W, Beccati M, Bourdeau P, et al. Efficacy of two formulations of afoxolaner (NexGard® and NexGard Spectra®) for the treatment of generalised demodicosis in dogs, in veterinary dermatology referral centers in Europe. Parasit Vectors 2018; doi.org/10.1186/s13071-018-3083-2.
Miller WH, Griffin CE, Campbell KL. Small Animal Dermatology, 7th ed. St. Louis, MO: Elsevier, 2013; 304-313.
Ravera I, Altet L, Francino O, et al. Small Demodex populations colonize most parts of the skin of healthy dogs. Vet Dermatol 2013; 24(1):168-172.
Ordeix L, Bardaqi M, Scarampella F, et al. Demodex injai infestation and dorsal greasy skin and hair in eight wirehaired fox terrier dogs. Vet Dermatol 2009; 20(4): 267-272.
Six RH, Becskei C, Mazaleski MM et al. Efficacy of sarolaner, a novel isoxazoline, against two common mite infectations in dogs: Demodex spp. and Otodectes cynotis. Vet Parasitol 222:62-66, 2016.
Tater KC, Patterson AP. Canine and feline demodicosis. Vet Med 2008; 103(8):444-461.
Scott DW, Miller WH, Griffin CE: Small Animal Dermatology. 5th edn. Philadelphia: W.B. Saunders Co., 1995; 417-432.
Zhou X, Hohman A, Hsu WH. Review of extralabel use of isoxazolines for treatment of demodicosis in dogs and cats. J Am Vet Med Assoc 2020; 256:1342-1346.

