1.7 Actinomycetic Infections – Small and Large Animals
Learning Objectives
- What are the etiologic agents of nocardiosis, actinomycosis and actinobacillosis?
- What are the clinical signs of nocardiosis, actinomycosis and actinobacillosis?
- What are the predisposing factors for an infection to be established?
- How do you diagnose nocardiosis, actinomycosis and actinobacillosis?
- How do you manage these three conditions?
- What do these diseases have in common regarding the etiologic agent and the clinical signs?
-
General Considerations
- Actinomycetic infections are caused by actinomycetes, which are filamentous or fungus-like bacteria.
-
- Examples of such infections include actinomycosis, actinobacillosis, and nocardiosis.
- The organisms causing most actinomycetic infections will induce the formation of mycetomas.
- Clinically, a mycetoma is characterized by the presence of tumefaction, draining tracts, and grains. The grains are very small, have different colors depending on the organism present and constitute agglomerations of microorganisms coated with host fibrin and immunoglobulins.
-
- Nocardiosis, actinomycosis and actinobacillosis will be discussed in this section.
-
Nocardiosis
-
-
Etiology:
- Nocardia asteroides, Nocardia brasiliensis, Nocardia otitidiscaviarum (formerly Nocardia caviae), Nocardia farcinica (agent of bovine farcy) and Nocardia nova (the main species infecting cats). These agents make up the Nocardia asteroides complex.
- Nocardia spp. organisms are intracellular, gram-positive, partially acid-fast, branching filamentous, cocobacillary aerobes.
- Nocardia spp. are common soil saprophytes that produce infection by wound contamination, inhalation, and ingestion, particularly in immunocompromised animals.
- The organisms have worldwide geographic distribution.
-
Clinical Signs:
- Bovine:
- Nocardia farcinica causes bovine farcy, which is a rare disease restricted to Africa, Asia, and South America.
- Skin lesions are characterized by firm, slow-growing, subcutaneous nodules that may ulcerate and drain a serous to purulent exudate, which may contain small white particles (“sulfur grains”). The nodules typically occur on the head, neck, shoulder, and limbs but can be found anywhere on the body. Lymphadenopathy is usually present.
- Bovine farcy can involve internal organs and result in death.
- Nocardia asteroides, Nocardia otitidiscaviarum, Nocardia farcinica and Nocardia Nova have been reported to cause mastitis in cattle. The infection typically occurs in one or two animals in a herd and lesions are characterized by edema, fibrosis, enlargement of the udder, draining tracts and presence of purulent discharge and white particles in the milk.
- Equine:
- Nocardia asteroides can rarely cause dermatitis in horses.
- Nocardiosis in horses commonly presents as a disseminated disease, which carries a poor prognosis. Affected horses often have other morbidities that compromise their immune system.
- Dogs and Cats:
- Lesions are characterized by cellulitis, ulcerated nodules, and abscesses that often develop draining tracts.
- Bovine:
-


-
-
-
- Lesions usually occur in areas of wounding, especially on the limbs and feet.
- Lymphadenopathy is often present.
- Cats frequently develop lesions on the ventral abdomen that resembles panniculitis or opportunistic mycobacterial infection.
- Pyothorax, fever, depression, dyspnea and neurologic signs may be present.
-
-
Diagnosis:
- History and clinical signs.
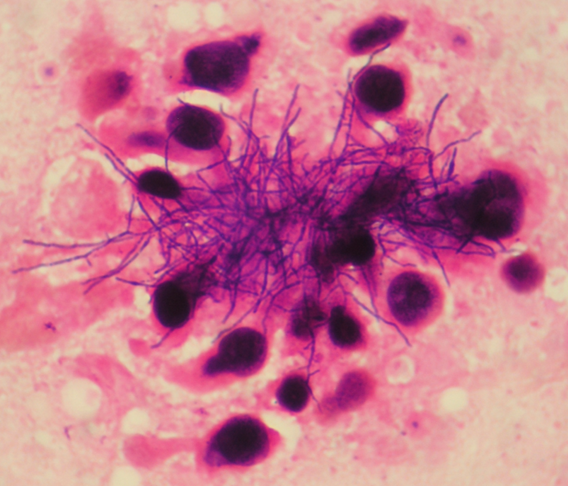
- Cytology from fine needle aspirates, or direct smears from exudate. Samples should be stained with Gram-stain (positive) or Giemsa stain.
-
-
-
- Aerobic culture (blood agar, Sabouraud agar, Lowenstein – Jensen agar).
- Biopsy – request Gram and acid-fast stains.
- Rapid identification of the etiologic agent can be done using molecular techniques.
-
Treatment:
- Surgical debridement and drainage.
- Ideally, antibiotic treatment should be chosen based on culture and sensitivity results. Inform the lab that you are suspecting of an actinomycetic infection.
- Drugs that can be effective empirically include potentiated sulfas, aminoglycosides and cephalosporines.
- Long-term therapy is required.
- Treatment must be continued for at least 1 month after clinical remission.
-
-
-
Prognosis:
- Guarded to poor for cases with systemic involvement. Typically good for cases limited to the skin.
-
-
Actinomycosis
-
General Considerations:
- Uncommon condition described in cattle, sheep, horses, goats, dogs and cats.
- In the U.S., actinomycosis has been reported mostly in the West and Midwest regions but it has a worldwide distribution.
- Actinomyces species normally inhabit the oral cavity, upper respiratory and digestive tracts.
- The organisms are opportunistic pathogens and invade damaged mucosa and skin.
- Examples of predisposing factors include mucosal damage caused by dietary roughage (large animals), exposure of dental alveoli when deciduous teeth are shed (large animals), and penetrating wounds of the skin.
-
Etiology:
- Actinomyces spp.
- The organisms are gram-positive, non-acid-fast, filamentous anaerobic rods.
-
Clinical Signs:
- Bovine:
- Actinomycosis is commonly seen in cattle.
- The main lesion is a rarefying osteomyelitis, which affects primarily the mandible and maxilla (lumpy jaw).
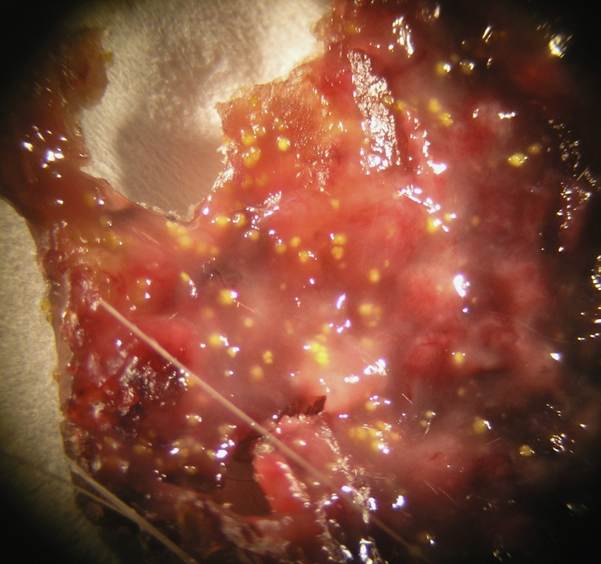
- Firm, immovable bony swellings extend to the overlying skin, resulting in nodules, abscesses and fistulae. The exudate is honey-like and contains hard, small, yellowish-white granules (sulfur granules). These lesions characterize a mycetoma (i.e. tumor, draining tracts, and granules).
- Bovine:
-

-
-
-
- The disease course may be rapid or progress over a period of years resulting in anorexia and emaciation.
- Swine:
- Actinomycosis in swine has been reported to affect the udder.
- Clinically, it is characterized by enlargement of the udder that may evolve to develop fistulous tracts, which discharge a yellowish purulent exudate containing sulfur granules (mycetoma).
- Trauma, including wounds caused by the teeth of suckling piglets, is thought to be a relevant predisposing factor.
- Horses, Sheep and Goats:
- Actinomycosis appears to be rare in horses, sheep, and goats.
- Clinical signs are similar to the disease in cattle (lumpy jaw).
- Dogs and Cats:
- Hunting or field dogs in Southern climates are predisposed.
- The lesion is characterized by a subcutaneous swelling or an abscess of the head, neck, thorax, and paralumbar or abdominal region.
- Osteomyelitis and empyema may occur.
- Draining tracts may discharge a thick, yellowish-gray or a thin, hemorrhagic exudate. The exudate is foul-smelling and may or may not contain sulfur granules (mycetoma).
-
-
Diagnosis:
- History and clinical signs.
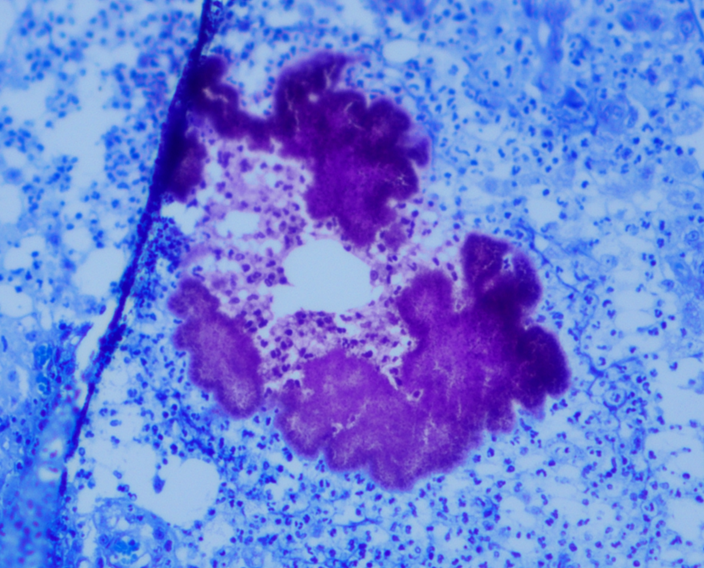
- Direct smears of fine needle aspirates, or direct smear of exudate from a draining tract.
- Biopsy – request special stains: Gram-stain or Brown-Brenn modified gram stain or Grocott’s methenamine silver.
- Tissue granules (sulfur granules) are found in approximately 50% of the cases.
- Anaerobic culture.
- Actinomycosis must be differentiated from nocardiosis. These diseases are very similar clinically.
-
Treatment:
- The most successful treatment is surgical excision or debridement with a long course of antibiotic therapy.
- Antibiotic therapy:
- Penicillin 80,000-100,000 IU/kg/day.
- Other antibiotic options include ampicillin, cephalosporins, chloramphenicol, and tetracycline.
- Antibiotic therapy is recommended for at least a month past clinical cure.
- Ideally, the antibiotic should be selected based on culture and susceptibility results. Inform the lab that you are suspecting of an actinomycetic infection.
- Treatment can last 3 to 4 months or more.
-
Prognosis:
- Guarded with reported relapses ranging from 15 to 42%.
-
-
Actinobacillosis
-
-
General Considerations:
- Actinobacillosis is more often seen in cattle and rarely in sheep, horses, swine, dogs and cats.
- It is worldwide in distribution. In the U.S., it is seen most commonly in the West and Southwest.
-
Etiology and Pathogenesis:
- The disease is caused by Actinobacillus lignieresii, which is a gram-negative, aerobic coccobacillus.
- The organism is a commensal found in the mouth of many animals but it can also be isolated from manure and soil.
- Actinobacillus lignieresii cannot invade healthy tissues and requires antecedent trauma such as sharp awns, stickers, or oral and cutaneous wounds.
-
Clinical Signs:
- Bovine:
- Actinobacillosis is most commonly seen in cattle.
- Subcutaneous, non painful abscesses are formed on the head (big head) especially at the area of cervical lymph nodes.
- Cervical lymph nodes are affected in the large majority of cases.
- The tongue can also be affected and will eventually appear enlarged, firm (wooden tongue) and will protrude.
- The abscessed lymph nodes are not warm to the touch and will eventually drain a thick, white to greenish exudate that contains brown-white granules (sulfur grains).
- The disease may extend to the pharynx and larynx resulting in dysphagia and dyspnea, respectively.
- Occasionally, the infection can disseminate and spread to the liver, lungs, gastrointestinal tract, and peritoneum, often resulting in death.
- Animals with tongue lesions have difficulties in apprehending and masticating food.
- Sheep:
- Actinobacillosis is a rare chronic granulomatous disease of sheep.
- It is characterized by cutaneous and subcutaneous abscesses that eventually become fibrotic.
- Areas most commonly affected are the cheeks, lips and nose but the head lymph nodes can also be involved.
- The lesions often drain a thick greenish-yellow purulent exudate, which contains sulfur granules.
- The tongue is not affected.
- Swine:
- The disease is rare and characterized by udder abscesses in sows.
- Horses:
- It is rare and can cause an enlarged tongue.
- Actinobacillus equuli can cause an often fatal septicemic disease in foals (shigellosis).
- Dogs and Cats:
- Single or multiple thick-walled abscesses of the head, neck, mouth, and limbs.
- The abscesses discharge a thick, white to green, odorless pus with soft yellow granules (mycetoma).
- Bovine:
-
Diagnosis:
- History and clinical signs.
- Direct smears of samples from fine needle aspirates.
- Biopsy – request special stains: Gram-stain or Brown-Brenn modified Gram stain).
- Tissue granules are usually present.
- Aerobic culture of purulent exudate.
-
Treatment:
- Bovine:
- 10 to 20% aqueous solution of sodium iodide IV at a dosage of 1g/15kg. Two or three injections at 10 to 14-day interval.
- Potassium iodide as an oral drench at 6 to 10g/head/day for 7 to 10 days.
- Ethylenediamine dihydroiodide (EDDI) in the feed at a dose of 15 to 30g/head/day for 2 to 3 weeks.
- Treatment should be discontinued if signs of iodism occur (anorexia, lacrimation, nasorrhea, or dry scaly skin and coat).
- Penicillin, streptomycin, tetracycline, chloramphenicol, and ampicillin can also be used.
- Triple sulfa (sulfanilamide, sulfapyridine, sulfathiazole) given IV at a dose of 1g/7kg for 5 to 6 days has been effective.
- Ideally, antibiotic should be based on culture and susceptibility results. Inform the lab that you are suspecting of an actinomycetic infection.
- Sheep:
- 10% aqueous solution of sodium iodine given IV or SC at the dose of 80 mg/kg or 20 to 25 ml/kg, weekly for 4 to 5 weeks.
- EDDI in the feed at the dose of 7.5 to 15g/head/day for 2 to 3 weeks.
- Streptomycin given IM at a dose of 20 mg/kg/day for 5 to 7 days works well when combined with systemic iodine therapy.
- Swine:
- Tetracycline has been reported to work well.
- Dogs and Cats:
- Sodium iodine at the dose of 20 mg/kg or 0.2 ml/kg of a 20% solution, orally q 12 h and high doses of streptomycin or sulfonamides.
- The organism is usually sensitive to tetracycline and chloramphenicol.
- Ideally, antibiotic should be based on culture and susceptibility results. Inform the lab that you are suspecting of an actinomycetic infection.
- All Species:
- Surgical extirpation or drainage and curettage are recommended.
- The course of the disease is long.
- Prognosis is guarded to poor especially when disseminated disease develops.
- Bovine:
-
Important Facts
- Nocardiosis, actinomycosis and actinobacillosis can all present clinically as a mycetoma (tumefaction, draining tracts, and grains).
- The organisms involved in actinomycosis and actinobacillosis are commensals found in the mouth and gastrointestinal tract of many healthy animals.
- Nocardia spp. organisms are common soil saprophytes.
- In all three conditions, trauma and wound contamination with the etiologic agents are necessary for infection to occur.
- In the three diseases, treatment includes surgical extirpation or drainage and curettage and long term antibiotic therapy.
- Treat for 1 month after clinical cure.
- Ideally, antibiotic should be based on culture and susceptibility results. Inform the lab that you are suspecting of an actinomycetic infection.
- Prognosis is guarded to poor for the three diseases.
References
Aitken ID. Diseases of Sheep. 4th ed. Ames, IO: Blackwell, 2007: 319.
Awad F I. Nocardiosis of the bovine udder and testis. Vet Rec 1960; 72: 341-342.
Bibernstein EL, Jang SS, Hirsh DC. Nocardia asteroides infection in horses: a review. J Am Vet Med Assoc 1985; 186: 273-7.
Howard JL. Actinobacillosis. In: Howard JL ed. Current Veterinary Therapy. Food Animal Practice. Philadelphia: WB Saunders Co, 1981;, 667.
Howard JL. Actinomycosis. In: Howard JL ed. Current Veterinary Therapy. Food Animal Practice. Philadelphia: WB Saunders Co, 1981;, 668.
Hutson LR. Actinomycosis in a sheep. Can J Comp Med 1939; 3:112-113.
Lewis EF. Penicillin therapy in actinomycosis in cattle. Vet Rec 1947; 59: 435.
Lloyd DH. Bovine Farcy. In: Howard JL ed. Current Veterinary Therapy. Food Animal Practice. Philadelphia: WB Saunders Co, 1981; 1136.
Miller WH, Griffin CE, Campbell KL. Small Animal Dermatology, 7th ed. St. Louis, MO: Elsevier, 2013; 212-214.Ribeiro MG, Salerno T, de Mattos-Guarald AL et al. Nocardiosis: An overview and additional report of 28 cases in cattle and dogs. Rev Inst Med Trop S. Paulo 2008; 50:177-185.
Rycroft AW and Garside LH. Actinobacillus species and their role in animal disease. The Vet J 2000; 159:18-36.
Scott DW. Bacterial Diseases. In: Large Animal Dermatology. Philadelphia, PA: W.B. Saunders, 1988; 146-150.

